Throat clearing can be a natural response to irritation or a symptom of an underlying condition. Some people may experience throat clearing due to thick or copious mucus
Complete Guide to Acid Reflux and GERD: Symptoms, Causes & Treatments
/in Throat Clearing /by Dr. Matthew OlesiakPost Nasal Drip: Symptoms, Causes, Treatment Options & More
/in Throat Clearing /by Dr. Matthew OlesiakPost nasal drip is a condition that can cause discomfort in the throat. It occurs when there is excess mucus in the body or when the body has difficulty clearing it.
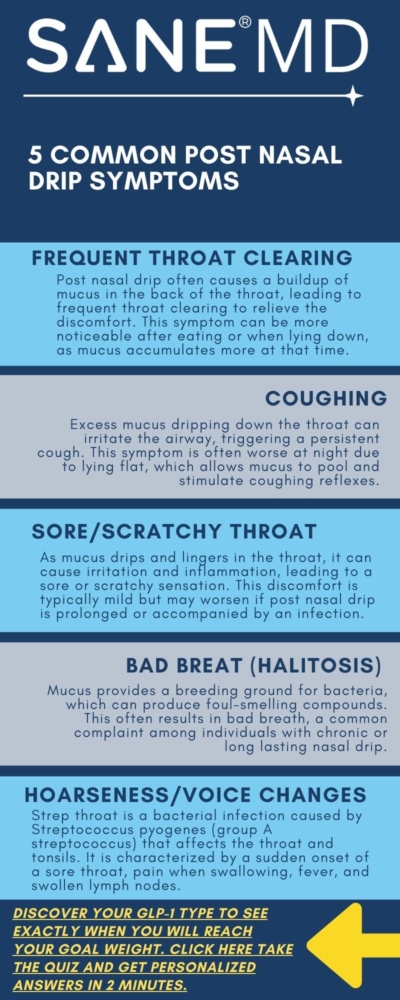
While mucus benefits the body, post nasal drip can lead to symptoms such as throat itchiness, coughing, frequent throat clearing, hoarseness, nausea, and bad breath.
Join us as we discuss the symptoms of postnasal drip, along with its causes and treatment options.
- Postnasal drip is a common condition that occurs when there is excess mucus production.
- Common symptoms of postnasal drip include frequent throat clearing or swallowing, cough, hoarseness, sore throat, nausea, and bad breath.
- Postnasal drip typically clears on its own, but there are over-the-counter and prescription medications that can help, as well as natural home remedies. See a medical doctor if your symptoms last longer than 10 days or are accompanied by a fever or mucus that has a foul odor.
Mucus Secretions: The Foundation of Post Nasal Drip
Everyone has experienced postnasal drip, but have you ever wondered why it occurs or how it is created? We have the answer for you.
The production of mucus by the nose, throat, and sinuses is a constant process that prevents the airways from drying out. Mucus has been found to serve an essential purpose in the human respiratory system. With its sticky surface, mucus can trap harmful particles such as germs, allergens, and dust, preventing their bodily entry. In addition, research has revealed that mucus contains abundant antiviral and antibacterial proteins that actively combat potential infections.
Typically, mucus goes unnoticed as it mixes with saliva throughout the day, and a person either swallows it or blows it out of their nose. However, excessive or thick production of mucus can cause it to become more noticeable, resulting in a sensation of the substance dripping down the back of the throat, which is medically referred to as a postnasal drip.
Postnasal Drip Symptoms
Common symptoms of postnasal drip include:
- Excess mucus in the throat
- Frequent throat clearing or swallowing
- A sore throat that may feel scratchy
- Nausea due to swallowing the excess mucus
- A cough, particularly if it worsens at night when lying down. Postnasal drip is often called “upper airway cough syndrome.”
- Halitosis (bad breath)
- Runny nose
- Hoarseness
- A burning sensation in your throat
- The feeling of a lump in the back of your throat
- Watery eyes
Causes of Post Nasal Drip
Postnasal drip can occur due to changes that cause mucus to thicken or become excessive.
Allergies are one of the most common causes of postnasal drip. For example, seasonal allergies triggered by pollen release from plants can cause the body to produce extra mucus to eliminate the pollen spores.
Cold weather or dry air can also lead to postnasal drip. Breathing in cold or dry air can irritate the nose and throat, prompting the body to create mucus to humidify and warm the passages, thus easing the irritation. Additionally, cold weather has links to viral infections such as the flu, sinus infections, and the common cold, all of which can cause symptoms of postnasal drip.
Furthermore, the body responds to invading germs by creating more mucus to flush them out. Although uncomfortable, postnasal drip shows the body’s efforts to stay healthy.
Other potential causes of post nasal drip include:
- Eating spicy foods
- Pregnancy
- Acid reflux or gastroesophageal reflux disease (GERD)
- Allergic rhinitis (an inflammation of the inside of the nose due to allergens, like pollen and dust)
- Sinusitis (inflammation of the mucous membranes that line the sinuses due to viral or bacterial infection, fungi, or allergies.)
- Chronic respiratory conditions, like chronic obstructive pulmonary disease and emphysema
- Specific medications, particularly some birth control prescription medications and those for blood pressure.
- Smoking or breathing secondhand smoke
- Hormone fluctuations
- Consuming dairy products
- Deviated septum, a condition that occurs when the bone that separates the nostrils is off-center
- Swallowing problems

How to Treat Post Nasal Drip
There are several ways to relieve post nasal drip. You can employ over-the-counter or home remedies to reduce postnasal drip symptoms or a combination. We’ll cover common over-the-counter medicines first.
Over-the-Counter Treatment Options
Specific over-the-counter (OTC) treatments can help if you have a sore throat, cough, or congestion along with postnasal drip. These treatments include:
- Cough lozenges to soothe a sore throat
- Acetaminophen products, like Tylenol, to ease sore throat pain and reduce fever
- Antihistamines to reduce allergy symptoms. Popular antihistamines include Benadryl and Claritin.
- Sudafed to ease congestions
- Robitussin Expectorant or Mucinex to loosen mucus
- Medicated nasal sprays, such as Afrin, to clear congested nasal passages
- Saline nasal spray to alleviate nasal congestion
- Nasal irrigation to flush out nasal passages. A neti pot is a popular nasal irrigation tool.
- Vapor rub applied to the chest, back, or throat to help clear congestion. A famous brand is Vicks VapoRub.
- Allergy shots to reduce your immune system’s adverse reaction to allergens
Prescription Medications
Postnasal drip can be treated with prescription medications that target the underlying cause.
Atrovent (ipratropium bromide) or a steroid may be prescribed for those with persistent or asthma-related symptoms. Antibiotics or antifungals may be necessary if the cause is a bacterial or fungal respiratory infection.
For GERD, a treatment plan involving medication and lifestyle changes is necessary. This may include avoiding fatty and spicy foods, taking acid-reducing medication, and sleeping with your head elevated (1).
Surgical Solutions
Surgery may be a solution if your postnasal drip is challenging to treat or caused by anatomical issues.
Surgeries can relieve postnasal drip caused by sinus issues, a deviated septum (septoplasty or submucosal resection), and nasal blockages.
Natural Home Remedies
There are some general lifestyle tips you can try to make dealing with postnasal drip easier, regardless of the cause.
- Drink lots of water. Water lubricates your throat and thins the mucus secretions. It also helps prevent dehydration.
- Rinse your nasal passages with a neti pot or other nasal irrigation tool, such as sinus rinses.
- Use a cool-mist humidifier at night while you sleep to moisturize your mouth, throat, and nasal passages.
- Sleep with your head slightly elevated to prevent mucus from gathering at the back of your throat
- Drink warm liquids, like tea or just plain water. You can also sip a mug of chicken broth or soup to help thin mucus.
- Use a HEPA vacuum to trap dust particles, which can help prevent an allergic reaction and resulting postnatal drip.
- Change air filters on your heating and air conditioning system regularly.
- Add a few drops of eucalyptus or peppermint essential oil to a diffuser to help relieve congestion.
- Use dust mite mattress covers and pillowcases to keep dust mites at bay.
When to Call a Doctor
Make an appointment with your doctor if you experience:
- Symptoms lasting at least 10 days
- Excess mucus that does not diminish despite using over-the-counter, prescription, and/or natural home remedies.
- Foul-smelling mucus
- If your symptoms accompany a high fever
- Trouble swallowing or breathing
- Shortness of breath
- Vomiting
- Ear pain
The symptoms above could indicate a bacterial infection that may require antibiotics. However, if it’s a viral infection, antibiotics won’t be effective, and a doctor won’t prescribe them.
In some cases, healthcare providers may suggest tests to determine the cause of the symptoms, which could include stomach acid reflux or nasal polyps. A steroid nasal spray may also be recommended for individuals with persistent allergies.
Summary
Postnasal drip is a common condition that can cause discomfort and irritation in the throat and difficulty swallowing. It is often triggered by environmental factors such as allergies, cold weather, or dry air.
Although it usually clears up without medication, antihistamines and decongestants can be helpful for those with viral infections or allergies.
If you experience persistent postnasal drip or other symptoms, it is best to consult with your doctor for proper diagnosis and treatment.
Frequently Asked Questions
What is post-nasal drip a symptom of?
Postnasal drip is a common symptom of cold, sinusitis, seasonal allergies, and cold weather or dry air. It can also be caused by eating spicy foods, eating dairy products, acid reflux, chronic respiratory conditions, certain medications, and swallowing problems.
What medication is used to dry up sinus drainage?
Various medications can aid in reducing sinus drainage in the throat. Decongestants work by reducing the sinuses’ swelling, thus lessening mucus production. Antihistamines can help reduce inflammation caused by allergies. Expectorants help to thin out the mucus, making it less sticky and easier to expel.
What is the quickest way to get rid of post nasal drip?
- Drink lots of water.
- Rinse your nasal passages with a neti pot.
- Use a cool-mist humidifier at night while you sleep to moisturize your mouth, throat, and nasal passages.
- Sleep with your head slightly elevated to prevent mucus from gathering at the back of your throat.
- Drink warm liquids, such as tea, or chicken soup, to help thin mucus
- Add a few drops of eucalyptus or peppermint essential oil to a diffuser to help relieve congestion.
Does Mucinex help stop post nasal drip?
If you’re suffering from excess mucus, drugs like Mucinex and Robitussin, which contain guaifenesin, may be helpful. Another option is to use a neti pot to rinse your nasal passages and clear away any excess mucus. Also, a humidifier can help moisten the air and alleviate your symptoms.
1- https://bmcprimcare.biomedcentral.com/articles/10.1186/s12875-021-01369-0
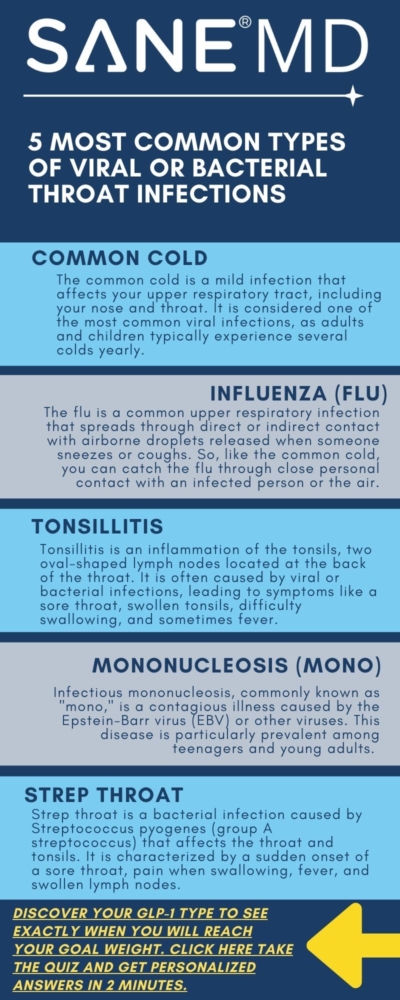
What are the Different Types of Throat Infections?
/in Throat Clearing /by Dr. Matthew OlesiakThroat infections are a common problem worldwide, causing discomfort and pain in the throat. They can also result in missed work, reduced pay, and increased medical expenses.
This comprehensive throat health blog will cover the different types of throat infections and their causes, symptoms, and treatment options to help alleviate the pain.
- It’s important to distinguish between viral and bacterial throat infections to receive appropriate treatment.
- Consider natural remedies like saltwater gargles, sucking on ice chips, using throat cleaners, and drinking warm liquids, or try over-the-counter treatments to alleviate symptoms.
- If your sore throat persists or is accompanied by severe symptoms or complications resulting from untreated bacterial infections, seek medical attention.
Throat Infections: The Basics
The throat (pharynx) serves many purposes. It transports food to the esophagus and air to the windpipe (trachea). It houses the voice box (larynx) that enables you to talk and the tonsils that fight off germs before they can reach other areas of the body.
A throat infection, also known as pharyngitis, may be caused by a viral or bacterial infection resulting in inflammation of the throat tissues. This inflammation leads to redness, pain, and swelling of the throat and accompanying structures, such as the tonsils.
Symptoms of a Throat Infection
Sore throat symptoms are typically present in a throat infection. Other symptoms of a throat infection usually include a burning sensation and pain in the throat, which can be mild or severe. Other throat structures, such as the tonsils, may also be affected.
There are often additional symptoms that vary depending on the cause. These symptoms may include:
- Difficulty swallowing
- Swollen lymph nodes in the neck
- Swollen, reddened tonsils
- Headache
- Cough
- Earache
- Hoarse voice or laryngitis
- Congestion
- Runny nose
- Fever and chills
- Body aches
- Fatigue
- Upset stomach
- Pus or white streaks in the throat or covering the tonsils
Types of Viral or Bacterial Throat Infections
While most throat infections are viral, some are caused by bacteria. Strep throat and scarlet fever are exclusively bacterial, while others can be caused by either. Here are some of the most common types of throat infections.
Cold
The common cold is a mild infection that affects your upper respiratory tract, including your nose and throat. It is considered one of the most common viral infections, as adults and children typically experience several colds yearly. Children are more prone to catching a cold than adults.
In total, over 200 different viruses can cause the common cold, but the most common type is rhinoviruses. These viruses are highly contagious and easily transmitted from person to person through close personal contact or by air. You can also contract the virus by touching an infected surface and then touching your eyes, mouth, or nose.
Symptoms of a cold typically include:
- Runny nose
- Congestion
- Sneezing
- Sore throat
- Stuffy nose
- Minor headache
- Slight fever
Influenza (flu)
The Centers for Disease Control and Prevention (CDC) defines the flu as “a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs. It can cause mild to severe illness, and at times can lead to death.” (1)
The flu is a common upper respiratory infection that spreads through direct or indirect contact with airborne droplets released when someone sneezes or coughs. So, like the common cold, you can catch the flu through close personal contact with an infected person or through the air. You can also get it by touching a surface, such as a phone or dish, that an infected person has used.
It’s important to note that influenza affecting the upper respiratory tract is not the same as the stomach flu viruses that cause vomiting and diarrhea.
Initially, the flu symptoms can be mistaken for a common cold, such as a runny nose, sneezing, and sore throat. However, colds typically have a gradual onset, while the flu comes on suddenly. Additionally, the flu tends to cause more severe symptoms than colds, resulting in greater discomfort.
Symptoms can include:
- Fever
- Headache
- Shortness of breath
- Dry cough that is persistent
- Sore throat
- Congested or runny nose
- Fatigue
- Muscle aches and weakness
Tonsillitis
Tonsillitis is a condition where the tonsils, a pair of tissue masses located at the back of the throat, become infected.
The tonsils are crucial in filtering germs that could enter the airways and cause an infection. They also produce antibodies to combat infections. However, when bacteria or viruses become too much for the tonsils to handle, they can become swollen and inflamed. This condition is more common in children than adults.
Tonsillitis can be caused by a viral infection or by bacteria.
Symptoms of tonsillitis include:
- Inflamed, swollen tonsils
- Yellow or white sections of the tonsils
- Sore throat (Sore throats are one of the most common symptom)
- Headache
- Swollen glands (lymph nodes) on the neck
- A hoarse, scratchy voice
- Pain while swallowing
- Bad breath
- Difficulty swallowing
Mononucleosis (Mono)
Infectious mononucleosis, commonly known as “mono,” is a contagious illness caused by the Epstein-Barr virus (EBV) or other viruses. This disease is particularly prevalent among teenagers and young adults, especially college students.
To avoid contracting mono, be careful when sharing personal items like toothbrushes or beverages, as it can be transmitted through saliva. Additionally, kissing someone infected with mono can also result in contracting the illness, which is why mono is known as the “kissing disease.”
Symptoms of mononucleosis include:
- Headache
- Body aches
- Severe fatigue
- Sore throat
- Swollen tonsils
- Rash
- Night sweats
- Swollen, tender lymph nodes in the neck and armpits
Strep Throat
Strep throat is a type of bacterial infection affecting the throat and tonsils. It is caused by group A streptococcus, also known as Streptococcus pyogenes.
This bacteria lives in the nose and throat and can quickly spread from an individual already carrying strep A bacteria or who is already infected with it.
While anyone can contract strep throat, it is commonly found in children and teenagers aged 5 to 15.
This condition can lead to complications such as kidney inflammation, rheumatic fever, and heart valve damage if left untreated. Symptoms of rheumatic fever include painful and inflamed joints, as well as a specific type of rash.
Symptoms include:
- Severe throat pain. (The sore throat usually starts suddenly.)
- Painful swallowing
- High fever
- Inflamed, swollen tonsils
- Swollen glands or lymph nodes in the front of the neck
- Small red spots on the roof of the mouth
- White streaks of pus on the tonsils
Scarlet Fever
Scarlet fever, also known as scarlatina, is an infection caused by group A Streptococcus bacteria – the bacteria that causes strep throat. The bacteria release a toxin that leads to a bright red rash spreading across the body, hence the name “scarlet” fever.
Only a tiny percentage of people who have strep throat develop scarlet fever.
Though rare, untreated scarlet fever can lead to severe complications, including pneumonia, sinus infection, pockets of pus (abscesses) near your tonsils or brain, rheumatic fever, arthritis, and kidney damage.
Symptoms of scarlet fever include:
- A red, bumpy rash all over your body
- Sore throat pain
- White coating on the tongue
- Red, swollen tonsils
- Fever
- Chills
- Swollen glands
- Stomach pain
- Body aches
- Decreased appetite
Treatments for Throat Infections
Prevention is critical when treating throat infections, but sometimes, they can still occur despite our best efforts.
If your sore throat is caused by a virus, the throat infection may go away on its own or can be treated effectively with timely intervention.
If your doctor suspects you have a throat infection, they will likely perform a throat culture by swabbing your throat for mucus or a fluid sample to be analyzed in a laboratory. This will help your doctor identify the cause of your infection.
Antibiotics for Bacterial Throat Infections
If you have strep throat or another bacterial throat infection, your doctor will prescribe antibiotics to kill the bacteria.
It is essential to finish all antibiotics prescribed, even if you start feeling well. If you don’t do so, your infection may take longer to heal. It may also recur and resist that medication, so your doctor may have to prescribe a stronger antibiotic.
Examples of popular antibiotics include penicillin and amoxicillin.
Pain Relievers for Head Pain, Body Aches, and Fever
Over-the-counter pain relievers, such as sprays, lozenges, or liquid gargles, can alleviate pain and fever and soothe inflammation.
Popular pain relievers include:
- Ibuprophen, a non-steroidal anti-inflammatory. Examples include Motrin and Advil
- Acetaminophen. Examples include Excedrin and Tylenol
- Medicated lozenges to soothe throat pain
- Antiseptic gargle solutions for sore throat.
Surgery
Tonsillitis is a type of throat infection that can spread to the tonsils.
If antibiotics do not work, one possible treatment option is surgically removing the tonsils, also known as a tonsillectomy.
Your doctor may suggest this procedure if you have abscesses on your tonsils that cannot be drained or if you experience a persistent bad taste or foul odor in your mouth despite taking antibiotics.
Natural Ways to Treat or Avoid Throat Infections
To Treat:
- Gargle with warm salt water several times a day to relieve throat pain
- Get plenty of rest
- Eat or drink chicken soup or warm liquids
- Drink warm liquids like tea.
- Suck medicated throat lozenges
- Drink lots of fluids to stay hydrated and avoid dehydration
- Eat ice cream or popsicles, or suck on ice chips to cool the heat in your throat
- Use a cool mist vaporizer at night while sleeping
To Avoid Giving or Contracting:
- Avoid sharing eating utensils, water glasses, toothbrushes, etc.
- Use alcohol-based hand sanitizers or wash your hands frequently throughout the day
- Use a sanitation agent to sanitize shared surfaces, such as phones, filing drawers, etc.
When to See a Doctor
You should see a healthcare provider if you:
- run a high fever for more than a couple of days
- experience trouble breathing
- develop a red skin rash
- symptoms are not getting better after 7-10 days
- see what streaks on your tonsils or the back of your throat
Summary
If you get a sore throat, it may be due to a viral or bacterial infection. The common causes of viral and bacterial infections include the cold, flu, strep throat, and mononucleosis.
Typical symptoms of throat infections include inflamed, swollen throat, trouble talking, and painful swallowing. Most sore throats and other signs of a throat infection resolve on their own. However, if it’s a sore throat caused by strep throat or mononucleosis, it may not clear without medical treatment.
It is recommended to seek medical attention if you have a throat infection. Although some conditions may resolve on their own, untreated infections can result in complications such as tonsillitis.
Doctors may prescribe antibiotics or specific pain relievers. You can also try home-care remedies such as using lozenges, sucking on ice chips, and using a humidifier.
1- https://www.cdc.gov/flu/about/keyfacts.htm