Contrave and Hydrocodone Drug Interactions: Risky Combo?
Dr. Matthew Olesiak, MD, is the Chief Medical Director at SANESolution, a renowned wellness technology company dedicated to providing evidence-based solutions for optimal living. Dr. Olesiak earned his medical degree from the prestigious Jagiellonian University Medical College in Kraków, Poland, where he developed a strong foundation in medicine.

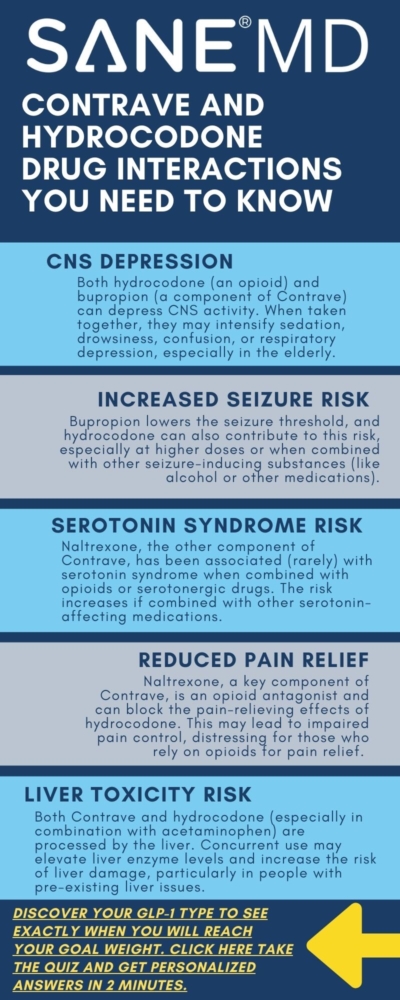
Combining medications can offer therapeutic benefits, but it can also increase the risk of serious side effects. One such potential interaction that has raised concerns is between Contrave and hydrocodone. While Contrave – an FDA-approved medication for chronic weight management, has helped certain individuals achieve clinically meaningful weight loss, its active components, naltrexone and bupropion, may interact dangerously with opioids like hydrocodone.
This article explores the possible Contrave and hydrocodone drug interactions, focusing on safety risks, underlying pharmacology, and what patients and healthcare providers need to know. Understanding this risky combo is crucial, especially for individuals with a history of opioid dependence, psychiatric illness, or conditions like bipolar disorder and seizure disorder.
Key Takeaways
- Combining Contrave and hydrocodone can trigger opioid withdrawal symptoms and increase the risk of seizures, making this interaction potentially dangerous.
- Contrave’s component naltrexone blocks opioid receptors, while bupropion lowers the seizure threshold, both contribute to heightened risk when used with opioids.
- Patients should consult their healthcare provider before combining Contrave with any other medications, especially opioids or over-the-counter drugs, due to the potential for serious adverse reactions.
Summary Table of Contrave and Hydrocodone Drug Interactions
| Interaction Aspect | Details |
|---|---|
| Primary Concern | Naltrexone blocks opioid receptors, while bupropion lowers the seizure threshold. Combining Contrave with hydrocodone can lead to serious adverse effects. |
| Opioid Withdrawal Risk | Sudden onset of withdrawal symptoms (e.g., nausea, anxiety, sweating, muscle aches) if opioids are still in the system when starting Contrave. |
| Seizure Risk | Bupropion increases seizure risk, especially with high doses or when combined with opioids, alcohol, or other CNS depressants. |
| Impact on Pain Relief | Hydrocodone may become ineffective due to opioid receptor blockade by naltrexone. |
| Neuropsychiatric Concerns | Increased risk of mood changes, hallucinations, and other serious neuropsychiatric adverse events. |
| Cardiovascular Effects | Contrave may raise blood pressure and heart rate. Interaction with hydrocodone could worsen cardiovascular instability. |
| Boxed Warning | Contrave includes a boxed warning advising against use in patients currently taking opioids or undergoing opioid withdrawal. |
| Recommendation | Do not take Contrave with hydrocodone or any opioid. Patients must be opioid-free for at least 7-10 days before starting Contrave. |
| Monitoring Required | Close monitoring by a healthcare provider is necessary if there’s any risk of opioid exposure or seizure susceptibility. |
What Is Contrave?
Contrave is a prescription medication approved for chronic weight management in certain obese patients or overweight adults with at least one weight-related condition, such as high blood pressure or type 2 diabetes.
It contains two active ingredients:
- Bupropion hydrochloride, an atypical antidepressant also used in smoking cessation treatment.
- Naltrexone, an opioid receptor antagonist originally used to treat opioid dependence and alcohol use disorder.
Together, naltrexone and bupropion (or bupropion naltrexone) target the brain’s reward and appetite centers, supporting behavior change and helping patients follow a reduced-calorie diet.
How Contrave Works
- Bupropion inhibits the reuptake of dopamine and norepinephrine, affecting the dopamine agonist effects involved in appetite and mood regulation.
- Naltrexone blocks opioid receptors in the brain, which may help reduce cravings and reward-driven eating.
But this unique mechanism also introduces risks, especially when other drugs are added to the mix.
Hydrocodone: An Opioid Painkiller
Hydrocodone is a widely prescribed opioid used for moderate to severe pain. It functions as a central nervous system depressant by binding to opioid receptors in the brain and spinal cord.
The presence of naltrexone in Contrave can block these receptors, making hydrocodone less effective and potentially triggering opioid withdrawal symptoms in dependent individuals.
Also, combining hydrocodone with bupropion therapy may increase the risk of seizures due to opposing effects on the central nervous system.
Contrave and Hydrocodone Drug Interactions
The combination of Contrave and hydrocodone is strongly discouraged due to the pharmacodynamic conflict between naltrexone bupropion and opioid medications. Hydrocodone, a commonly prescribed opioid for pain, relies on mu-opioid receptors to produce analgesia and euphoria.
Naltrexone, a key component in Contrave, is an opioid antagonist that blocks these receptors, while bupropion carries a significant risk of lowering the seizure threshold.
When these substances are taken together, the result can be a cascade of adverse reactions ranging from ineffectiveness of pain relief to potentially life-threatening complications like opioid withdrawal and seizures.
1. Opioid Withdrawal
Naltrexone binds competitively to opioid receptors and can displace opioids like hydrocodone, abruptly halting their effect.
This interaction can lead to the sudden onset of opioid withdrawal symptoms, which may include:
- Restlessness and anxiety
- Nausea, vomiting, and diarrhea
- Excessive sweating and chills
- Muscle cramps and body aches
- Increased heart rate and blood pressure
For individuals with even mild or recent opioid dependence, this reaction can be intense and debilitating.
The symptoms of opioid withdrawal typically begin within minutes to hours after taking Contrave if hydrocodone is still present in the body.
Dr. Matthew Olesiak, MD, Chief Medical Director at SANE MD, emphasizes:
“Taking naltrexone while opioids are still in the body can precipitate an abrupt and severe withdrawal reaction. Patients must be opioid-free for at least 7-10 days before starting Contrave.”
Because of this, the medication guide for Contrave explicitly advises patients and clinicians to confirm opioid abstinence before initiating treatment. The boxed warning alerts doctors to the dangers of combining opioid use with naltrexone systemic exposure.
For patients unknowingly using hydrocodone or those who take over-the-counter drugs with opioid-like effects, unintentional opioid withdrawal remains a real concern. This underlines the importance of full medication disclosure and complete screening before starting Contrave treatment.
2. Increased Risk of Seizures
The second major concern in this drug combination involves bupropion, an atypical antidepressant and dopamine-norepinephrine reuptake inhibitor that is known to lower the seizure threshold.
When combined with opioids, or in patients with certain medical histories, the risk of seizures increases substantially.
This risk is dose-related, meaning higher bupropion doses or rapid titration of Contrave increase the likelihood of convulsions.
The FDA has reported seizure incidence rates of approximately 0.1% at recommended doses, but this number rises with co-use of other drugs, misuse, or predisposing conditions such as:
- A personal or family history of seizure disorder
- History of head trauma or brain tumor
- Eating disorders like bulimia or anorexia nervosa
- Concurrent use of alcohol, systemic corticosteroids, or stimulants
- Use of other medications that affect central nervous system excitability
Combining hydrocodone and Contrave exacerbates these dangers.
Opioids can alter respiratory patterns and oxygen levels, potentially destabilizing brain function and further reducing the seizure threshold.
This is especially critical in patients taking bupropion for smoking cessation or to treat depression, where baseline seizure risk may already be elevated due to medication load or underlying conditions.
3. Blood Pressure Concerns
Another pressing issue in the interaction between Contrave and hydrocodone is their combined effects on the cardiovascular system. Contrave treatment has been associated with increases in both systolic and diastolic blood pressure, particularly in the early stages of use. While this elevation is generally mild, it may be dangerous for individuals with high blood pressure, severe hepatic impairment, or known cardiovascular disease.
The mechanisms behind this rise in blood pressure include the stimulant-like action of bupropion, which can increase sympathetic nervous system activity, and naltrexone, which may amplify these effects in susceptible individuals. When hydrocodone is added to the mix, its central nervous system depressant properties can cause unpredictable interactions, especially with heart rate and respiratory patterns.
In some cases, this can result in:
- Hypertensive episodes
- Heart palpitations
- Chest discomfort
- Fluctuations in oxygen saturation or blood carbon dioxide levels
Dr. Olesiak notes:
“Contrave can raise blood pressure and heart rate, so close monitoring is crucial for patients on hypertensive medications or with preexisting cardiovascular conditions.”
Because many individuals pursuing chronic weight management may already be managing high blood pressure, obese patients must be evaluated carefully before initiating therapy. Regular monitoring is recommended, especially during the start of Contrave treatment, to ensure a safe cardiovascular response.
Clinicians are advised to adjust treatment based on individual risk factors and, when necessary, reduce the dose or modify the timing of extended-release tablets to minimize peaks in systemic exposure.
Additional Risks and Considerations
While the most prominent dangers of combining Contrave and hydrocodone involve opioid withdrawal and seizures, there are several other drug interaction concerns that warrant equal attention. From allergic responses to systemic complications, these interactions can present suddenly and with serious consequences, particularly in patients with predisposing health factors or those taking other medications.

Risk of Allergic Reaction
Using multiple medications, especially those that act on the central nervous system or immune pathways, can increase the likelihood of a severe allergic reaction. Individuals taking Contrave, especially when combined with opioids like hydrocodone, should be alert to early signs of hypersensitivity, which may include:
- Skin rash or hives
- Itching or swelling, particularly around the face, lips, or throat
- Wheezing, difficulty breathing, or tightness in the chest
These symptoms may indicate a systemic allergic reaction requiring emergency medical attention. While rare, allergic responses may result from either the naltrexone bupropion formulation itself or from a Contrave interaction with another agent, prescription, or otherwise.
Because opioids like hydrocodone are known to release histamine in some users, co-use with Contrave can amplify this response and potentially increase the risk of an allergic cascade. Individuals with a history of drug sensitivities should inform their healthcare provider before starting Contrave treatment or combining it with other drugs.
Adverse Reactions and Side Effects
The FDA has issued clear warnings about the adverse reactions associated with combining Contrave with other drugs that lower the seizure threshold, such as hydrocodone. This combination may increase the risk of serious neuropsychiatric adverse events, including:
- Agitation, mood swings, and emotional instability
- Disorientation, delusional thinking, or hallucinations
- Panic attacks or suicidal ideation
- Cardiovascular symptoms like rapid heartbeat or chest pain
These side effects may emerge more rapidly or with greater severity when Contrave is combined with opioids, alcohol, or systemic corticosteroids, all of which can interact with the bupropion naltrexone mechanism.
In placebo-controlled trials, patients treated with Contrave reported adverse reactions such as:
- Nausea (especially in the early weeks of treatment)
- Dizziness, light-headedness, or blurred vision
- Insomnia, anxiety, or vivid dreams
- Elevated blood pressure and heart rate
These findings are detailed in a randomized, phase 3 trial published in Obesity, which evaluated the safety and efficacy of naltrexone sustained-release (SR) and bupropion SR combination therapy. The study reported that the most common adverse event was nausea, which was generally mild to moderate and transient. Additionally, there were minimal changes in blood pressure from baseline and a 1 bpm increase in pulse rate with the combination therapy.
Importantly, these side effects were more pronounced in individuals who consumed high-fat meals prior to dosing or who exceeded the recommended bupropion doses.
Healthcare professionals should take extra care when evaluating patients for Contrave, particularly if they are taking multiple medications or have a psychiatric or cardiovascular history.
Seizure Threshold and Risk Factors
A central concern with Contrave is its impact on the seizure threshold. Bupropion therapy inherently reduces this threshold, making seizures more likely in vulnerable individuals, especially when other substances are present.
Certain risk factors dramatically increase the likelihood of experiencing a seizure during contrave treatment:
- History of seizures or previous unexplained fainting spells
- Presence of a brain tumor or recent head injury
- Use of medications like systemic corticosteroids that alter electrolyte balance
- Underlying metabolic disturbances (e.g., low blood sugar)
- Suddenly stopping alcohol or benzodiazepines after prolonged use
Contrave’s medication guide specifically warns against alcohol use during treatment, as it can both increase the risk of seizures and trigger opioid withdrawal symptoms if co-occurring use is involved.
According to Dr. Matthew Olesiak, MD:
“Patients who use alcohol chronically or are tapering off sedatives must be evaluated for seizure vulnerability before initiating any therapy that includes bupropion.”
Also, there is evidence that patients withdrawing from long-term smoking cessation treatment or sedative hypnotics may experience temporary neurological instability, which could further reduce the seizure threshold.
For this reason, it is critical to monitor patients during the initial phases of Contrave dosing, particularly if they are managing concurrent behavioral or substance-related disorders.
How Contrave Interacts With Other Drugs
The risk of Contrave interactions extends well beyond opioids. Because Contrave contains naltrexone and bupropion, both of which have broad pharmacological activity, the potential for certain drug interactions is significant. These interactions can modify the drug’s effectiveness, increase the likelihood of adverse reactions, and, in some cases, lead to serious or even life-threatening consequences.
Patients often take Contrave alongside other medications for chronic health conditions such as depression, high blood pressure, or diabetes. As a result, careful consideration of concomitant treatment is essential.
1. Monoamine Oxidase Inhibitors (MAOIs)
One of the most dangerous interactions involves monoamine oxidase inhibitors, a class of antidepressants that affect neurotransmitter metabolism. Using MAOIs, liked Nardil within 14 days of starting or stopping Contrave can result in hypertensive crises due to excessive norepinephrine stimulation caused by bupropion exposure.
These crises may present as:
- Sudden, severe headache
- Nausea or vomiting
- Rapid heart rate and chest pain
- High blood pressure spikes requiring emergency care
Our complete guide can help you determine how long Contrave stays in your system.
MAOIs are typically prescribed less frequently today, but their long-lasting effects mean patients must still be screened for any recent use before initiating Contrave treatment.
2. Other Antidepressant Drugs
Contrave may interact with other antidepressant drugs, especially those that influence the serotonergic neurotransmitter system. While bupropion itself is not a serotonergic agent, combining it with SSRIs, SNRIs, or tricyclics can increase the risk of serotonin syndrome, particularly in patients with major depressive disorder. These antidepressant drugs that may interact with Contrave include Zoloft, Paxil, Prozac, Lexapro, and Effexor.
Serotonin syndrome occurs when too much serotonin builds up in the brain and may lead to:
- Agitation, restlessness, or confusion
- Rapid heart rate and fluctuating blood pressure
- Muscle twitching or tremors
- Fever and profuse sweating
Because these effects overlap with symptoms of neuropsychiatric adverse events, prompt recognition is essential. Patients treated with both Contrave and serotonergic medications should be closely monitored by their healthcare provider, especially when starting Contrave treatment or when there are any dosage changes.
3. Smoking Cessation Aids
Another area of concern is the use of Contrave alongside smoking cessation aids, particularly those that contain bupropion hydrochloride. Medications like Wellbutrin for depression and Zyban, used for smoking cessation treatment, share the same active compound as part of the naltrexone bupropion combination in Contrave.
Taking both simultaneously can result in bupropion doses exceeding the recommended threshold, significantly increasing the likelihood of:
- Seizure disorder activation due to compounded central nervous system stimulation
- Adverse reactions such as insomnia, irritability, or elevated blood pressure
- Increased risk of serious neuropsychiatric adverse events, particularly in patients with a psychiatric illness
Because of the shared mechanism, healthcare providers should inquire about any past or present use of bupropion-containing products before initiating Contrave. Patients must also avoid unintentional duplication of therapy from over-the-counter drugs or compounded treatments that may include bupropion derivatives.
4. Drugs That Lower the Seizure Threshold
As discussed in prior sections, any other drugs that lower the seizure threshold can interact dangerously with bupropion.
These include:
- Antipsychotic medications (e.g., clozapine, risperidone)
- Corticosteroids
- Stimulants (e.g., amphetamines)
- Alcohol or withdrawal from alcohol/sedatives
- Antibiotics known to lower seizure threshold (e.g., quinolones)
Combining any of these with Contrave may increase the risk of seizures, especially in patients treated with high bupropion doses or those with risk factors such as prior seizures, eating disorders, or severe hepatic impairment.
5. Drugs That Affect Blood Pressure or Heart Rate
Many commonly prescribed drugs, including those for high blood pressure, anxiety, or asthma, can influence cardiovascular function. Since Contrave treatment may cause modest increases in blood pressure and pulse, combining it with other stimulants or medications affecting cardiac rhythm may increase the risk of complications like:
- Tachycardia
- Chest pain
- Arrhythmias or palpitations
- Hypertensive emergencies in sensitive individuals
For this reason, patients should be monitored closely when using Contrave with beta-blockers, decongestants, or medications for chronic weight management that contain sympathomimetic agents.
In summary, Contrave can interact with a wide variety of other medications, and some interactions carry serious risks. It’s critical for patients and prescribers to perform a complete medication review before starting treatment. Doing so can help prevent unexpected adverse reactions, support safe use of naltrexone bupropion, and ensure that the medication supports, not compromises, overall health goals.
Contraindications and Warnings
Avoid Contrave If You Have:
- Severe hepatic impairment
- Severe renal impairment
- Uncontrolled high blood pressure
- Seizure disorder
- Current or recent use of opioids
For patients with moderate hepatic impairment, dosage adjustment may be necessary to reduce systemic exposure and lower the risk of toxicity.
Weight Loss with Contrave: What the Research Shows
Contrave has demonstrated effectiveness in weight loss when combined with a reduced-calorie diet and lifestyle changes. In clinical trials, certain patients saw significantly greater weight reductions compared to placebo.
- Obese patients with an initial body mass index over 30 achieved meaningful results.
- Individuals also saw benefits in blood sugar control, appetite suppression, and metabolic health.
In a phase 3 clinical trial published in The Lancet, participants treated with naltrexone 32 mg plus bupropion experienced an average weight loss of 6.1% of their initial body weight over 56 weeks, compared to 1.3% in the placebo group. Additionally, 48% of those in the naltrexone-bupropion group achieved at least a 5% reduction in body weight, whereas only 16% of the placebo group reached this milestone.
However, results varied by patient and were affected by bupropion doses, high-fat meals, and preexisting conditions such as bipolar disorder or major depressive disorder.
Special Populations and Precautions
Breastfeeding and Pregnancy
- Breast milk may contain trace amounts of Contrave ingredients. Use during breastfeeding is not recommended.
- Not enough data exists on the effects of Contrave during pregnancy. Risks must be weighed against the benefits of Contrave treatment.
Children and Adolescents
Contrave is not approved for individuals under 18 years of age due to unknown effects on brain development and a higher risk of neuropsychiatric adverse events.
Psychiatric Illness
People with psychiatric illness, including depression or bipolar disorder, require careful monitoring. There is a boxed warning that alerts doctors about the increased risk of suicidal thoughts and behaviors in young adults taking antidepressant drugs like bupropion.
Tips for Patients and Providers
- Always consult a healthcare provider before starting or stopping Contrave or opioids.
- Do not take Contrave if you are currently using opioids or undergoing treatment for opioid withdrawal.
- Talk with your doctor about other drugs or over-the-counter drugs you are taking, including herbal supplements.
- Avoid alcohol while on Contrave, and never suddenly stop drinking alcohol without medical guidance.
- Report any signs of allergic reaction, such as skin rash, swelling, or difficulty breathing, immediately.
Frequently Asked Questions (FAQ)
When starting a medication like Contrave, patients often have questions about safety, especially when other medications, like opioids or painkillers, are already in use.
Below are some of the most common concerns related to Contrave interactions, particularly with hydrocodone, other drugs, and pain relief medications in general.
1. Can you take Contrave with hydrocodone?
It is not recommended to take Contrave with hydrocodone. Contrave contains naltrexone, which blocks opioid receptors and can trigger sudden opioid withdrawal symptoms in anyone with recent or ongoing opioid use.
Also, bupropion, the second ingredient in Contrave, lowers the seizure threshold, making the combination even riskier. Patients must be opioid-free for at least 7-10 days before starting Contrave, as noted in its medication guide and boxed warning alerts.
Always consult your healthcare provider before combining these medications.
2. What happens if you take opioids with Contrave?
Taking opioids like hydrocodone while on Contrave can lead to severe adverse reactions. The naltrexone in Contrave blocks the opioid’s effect, which may result in ineffective pain relief and can also cause sudden, intense opioid withdrawal symptoms such as nausea, muscle aches, sweating, and anxiety.
If taken together unintentionally, the patient may experience an increased risk of complications requiring medical intervention. This interaction can also raise blood pressure and contribute to other serious neuropsychiatric adverse events.
Patients with a history of opioid dependence or chronic opioid use should avoid Contrave unless medically cleared.
3. Can you take hydrocodone and bupropion together?
Taking hydrocodone and bupropion together is generally discouraged due to the increased risk of seizures. Bupropion inhibits the reuptake of dopamine and norepinephrine and lowers the seizure threshold, especially when combined with substances that depress the central nervous system, such as opioids.
This combination may also result in unpredictable adverse reactions, including mood disturbances and respiratory complications.
If these drugs are prescribed together, it should be done under close medical supervision with appropriate dosage adjustment and monitoring. Discuss any existing health conditions, including seizure disorder, with your healthcare provider.
4. What medications should I avoid with Contrave?
There are several other drugs that should be avoided while taking Contrave. Contrave drug interactions include opioids, monoamine oxidase inhibitors (MAOIs), and other antidepressant drugs that can increase the risk of serotonin syndrome or seizure disorder. Dangerous drug interactions can occur with various epilepsy medications, such as Tegretol.
Patients should also avoid over-the-counter drugs, such as cold medications containing stimulants, and other weight loss treatments or smoking cessation aids that contain bupropion hydrochloride. Use of alcohol, sedatives, or systemic corticosteroids can further increase the chance of seizures or adverse reactions.
Always inform your healthcare provider of all prescription and nonprescription medications you take before starting Contrave treatment.
5. Can you take painkillers with Contrave?
Some non-opioid painkillers may be used with Contrave, but opioid-based medications like hydrocodone should be avoided due to the naltrexone bupropion combination. Naltrexone systemic exposure blocks the effect of opioids and may trigger opioid withdrawal, while bupropion doses can amplify seizure risk.
Safe alternatives for pain management may include acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), depending on your individual health profile.
Because certain drug interactions can be dangerous, your doctor must evaluate whether pain relief options are compatible with Contrave treatment. Never self-medicate while on Contrave without professional guidance.
Conclusion
The combination of Contrave and hydrocodone poses significant safety concerns due to the nature of their pharmacological effects. The naltrexone bupropion formula may trigger opioid withdrawal symptoms, elevate blood pressure, and increase the risk of seizures, especially in patients with underlying risk factors or preexisting conditions.
Understanding how Contrave interacts with other medications is critical for anyone pursuing chronic weight management. Always discuss Contrave interactions and any potential adverse reactions with your healthcare provider.
References