Modafinil and Contrave Drug Interactions: Safety Guide
Dr. Matthew Olesiak, MD, is the Chief Medical Director at SANESolution, a renowned wellness technology company dedicated to providing evidence-based solutions for optimal living. Dr. Olesiak earned his medical degree from the prestigious Jagiellonian University Medical College in Kraków, Poland, where he developed a strong foundation in medicine.

As more patients seek comprehensive approaches to improve focus, manage weight, and combat fatigue, the combination of medications like Contrave and modafinil is becoming increasingly common. However, this trend raises important safety concerns. The interaction between these two medications is not widely studied in clinical trials, making careful consideration and medical guidance essential for anyone considering or currently using both.
This guide examines the known and potential modafinil and Contrave drug interactions, highlights the increased risk of side effects, and provides guidance on monitoring, dosage adjustment, and risk factors.
Key Takeaways
- Combining Contrave and modafinil may increase the risk of seizures, serotonin syndrome, and elevated blood pressure. Monitoring is critical for patients on both medications.
- Contrave contains bupropion and naltrexone—two active compounds with unique effects on the brain’s reward system, which may intensify adverse reactions when combined with modafinil.
- Physicians must weigh the therapeutic benefits of this combination against potential complications, especially for patients with a history of psychiatric disorders, substance use, or cardiovascular conditions.
Understanding Contrave and Modafinil
Contrave is a fixed-dose combination medication composed of two active ingredients: bupropion and naltrexone. Together, they offer a unique dual mechanism of action aimed at addressing the neurochemical drivers behind overeating and cravings. Approved by the FDA for chronic weight management, Contrave is prescribed for certain adults with an initial body mass index (BMI) of 30 or higher, or 27 and above if the patient also has a weight-related condition such as diabetes mellitus, high cholesterol, or hypertension.
The first component, bupropion, is an atypical antidepressant most commonly used in treating major depressive disorder and smoking cessation. It works by inhibiting the reuptake of dopamine and norepinephrine—key neurotransmitters in the brain’s reward system. Through this action, bupropion can reduce the psychological urge to eat for comfort or reward.
The second ingredient, naltrexone hydrochloride, is an opioid receptor antagonist typically used to treat alcohol and opioid addiction. By blocking opioid receptors in the brain, naltrexone dampens the pleasure response associated with certain behaviors—like eating highly palatable foods. This makes it easier for compatible patients to resist cravings, particularly during the early phase of a reduced-calorie diet.
Together, bupropion naltrexone produces therapeutic effects that extend beyond simple appetite suppression. The combination aims to rebalance disrupted brain signaling related to reward and self-control, allowing for more sustainable weight loss among certain obese adults or those with weight-related comorbidities.
Modafinil, in contrast, is a wakefulness-promoting agent. It is FDA-approved for the treatment of excessive daytime sleepiness associated with narcolepsy, shift work sleep disorder, and obstructive sleep apnea. Unlike traditional stimulants, modafinil does not have a direct amphetamine-like mechanism. Instead, it enhances dopaminergic effects by inhibiting the dopamine transporter receptor, resulting in increased extracellular dopamine levels in key areas of the brain that govern alertness and attention.
Although not approved for this purpose, modafinil is sometimes used off-label to assist with weight loss due to its energy-boosting and appetite-suppressing effects. Some individuals report that it reduces the urge to snack or overeat, especially when combined with calorie restriction. However, this off-label use carries potential safety concerns—particularly when modafinil is used alongside medications that already affect the central nervous system, such as Contrave.
Both drugs target overlapping neural circuits, which is part of what raises red flags about modafinil and contrave drug interactions. Since they can influence reward, motivation, energy, and mood, their combined use may lead to amplified effects—or unintended complications.
Modafinil and Contrave Drug Interaction Summary
Combination Overview, Risks, and Monitoring Considerations
| Category | Details |
|---|---|
| Drugs Involved | Modafinil and Contrave (bupropion/naltrexone) |
| Primary Concerns | Increased risk of seizures, elevated blood pressure, serotonin syndrome, and mood instability |
| CNS Impact | Both modafinil and bupropion influence dopamine and norepinephrine; overlapping mechanisms may amplify stimulation and lower seizure threshold |
| Serotonin Syndrome Risk | Potential risk when combined with serotonergic agents; modafinil and bupropion may contribute indirectly |
| Cardiovascular Risks | May cause hypertension, chest pain, and cardiac strain—especially in patients with obesity, heart disease, or high blood pressure |
| Mental Health Concerns | May increase agitation, insomnia, anxiety, or mood swings; greater risk in patients with bipolar disorder, OCD, or history of suicidal ideation |
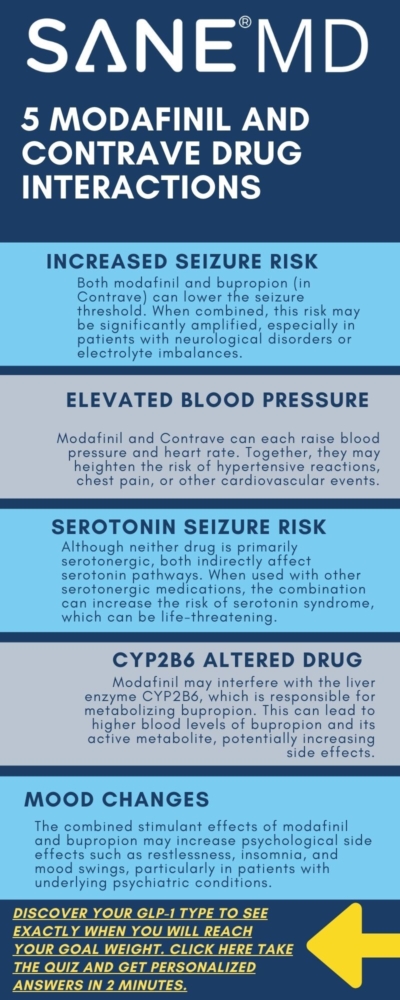
| Drug Metabolism Interaction | Modafinil affects CYP2B6, possibly altering bupropion and hydroxybupropion levels; may raise blood concentration and side effect risks |
| Contraindicated Medications | Opiate agonists (e.g., codeine, morphine), monoamine oxidase inhibitors (MAOIs) |
| Caution With | Tricyclic antidepressants, SSRIs, SNRIs, systemic corticosteroids, hormonal contraceptives |
| Common Side Effects (Combined) | Headache, nausea, abdominal pain, joint pain, insomnia, restlessness/anxiety |
| Serious Adverse Reactions | Seizures, hypertensive crisis, serotonin syndrome, manic episodes, chest pain |
| Monitoring Recommendations | Monitor blood pressure, mood changes, and signs of serotonin syndrome or seizure activity; regular check-ins advised |
| Dosing Guidelines | Gradual titration recommended; avoid high-fat meals with Contrave; dose adjustments may be necessary |
| Patient History Warnings | Assess for opioid use, alcohol dependence, psychiatric conditions, and use of other serotonergic or CNS-acting drugs |
| Off-Label Use Considerations | Modafinil may be used off-label for weight loss and attention; increased interaction risk if also used for smoking cessation or with additional CNS-active medications |
| Doctor Quote | “Combining stimulant-like medications can elevate the risk of seizures and increased blood pressure, particularly in individuals with underlying psychiatric disorders or cardiovascular issues.” – Dr. Matthew Olesiak, MD |
Why Combining These Medications Raises Concerns
While there is only limited data on modafinil and Contrave drug interactions, their shared impact on the central nervous system warrants caution. Both bupropion and modafinil influence neurotransmitters like dopamine and norepinephrine, potentially increasing stimulation beyond a safe threshold.
According to Dr. Matthew Olesiak, Chief Medical Director at SANE MD,
“Combining stimulant-like medications can elevate the risk of seizures and increased blood pressure, particularly in individuals with underlying psychiatric disorders or cardiovascular issues.”
Additionally, bupropion inhibits the reuptake of dopamine and norepinephrine, and modafinil further enhances dopaminergic activity. This overlapping effect can raise systemic exposure and heighten the chance of serotonin syndrome, particularly when combined with other drugs affecting the serotonergic neurotransmitter system.
Increased Risk of Seizures
Among the most serious risks of combining these medications is the seizure threshold being lowered. Patients receiving bupropion, especially those with preexisting neurological conditions or electrolyte imbalances, are at higher risk. Modafinil may further compromise this threshold.
“Modafinil’s stimulation of the brain’s dopamine system may synergize with bupropion therapy in a way that reduces the seizure threshold significantly,” says Dr. Olesiak.
Cardiovascular Effects and Blood Pressure Monitoring
Both bupropion naltrexone and modafinil may cause increased blood pressure and chest pain, particularly in obese patients or those with congestive heart failure. Because Contrave can cause hypertensive reactions, and modafinil may also elevate blood pressure, patients must be monitored carefully for signs of cardiac strain. Sudden onset of joint pain, abdominal pain, or chest pain may occur and should be reported immediately.
A dosage adjustment or dose reduction may be needed if patients experience high blood pressure during treatment.
Impact on Mental Health
Patients with bipolar disorder, major depressive disorder, or obsessive-compulsive disorder should approach this combination with extreme caution. The stimulant effects of modafinil may exacerbate mood instability, while initiating bupropion therapy in such individuals has been associated with suicidal ideation and manic episodes.
Moreover, the combined use of these drugs may increase agitation, insomnia, and anxiety. These adverse reactions may occur in individuals without prior psychiatric diagnoses, especially if no dose adjustment is made over time.
Risk of Serotonin Syndrome
While serotonin syndrome is more commonly associated with the use of SSRIs, SNRIs, and monoamine oxidase inhibitors, it’s important to recognize that serotonin syndrome occurs when multiple medications—especially those that influence the serotonergic neurotransmitter system—lead to excess serotonin in the brain. This can happen even when the medications involved are not classified as traditional serotonergic drugs.
Both bupropion and modafinil have indirect effects on serotonin pathways. Bupropion inhibits the reuptake of norepinephrine and dopamine, and while it is not a primary serotonergic agent, it may still interact with other drugs that act on serotonin systems, raising the overall risk. Modafinil, though primarily known for its dopaminergic effects, has been shown to influence multiple neurotransmitters, including serotonin, especially when used alongside other drugs with serotonergic properties.
When these medications are combined—either with each other or with SSRIs, SNRIs, tricyclic antidepressants, or monoamine oxidase inhibitors—there is a theoretical and documented risk of serotonin syndrome, as demonstrated in Science Direct. Symptoms may include agitation, confusion, rapid heart rate, high blood pressure, tremor, muscle rigidity, and, in severe cases, seizures or respiratory depression. These reactions may occur rapidly and require immediate medical attention.
Because neither bupropion nor modafinil is traditionally flagged as a high-risk serotonergic agent, serotonin syndrome can be under-recognized in clinical settings. Healthcare providers should remain vigilant when prescribing these drugs in combination with other serotonergic agents or in patients with a history of psychiatric disorders, bipolar disorder, or obsessive-compulsive disorder, where polypharmacy is common.
Drug Interactions with Opiates, Alcohol, and Other Substances
Bupropion naltrexone is contraindicated with opiate agonists, such as morphine and codeine. Naltrexone, as an opioid antagonist, can precipitate opioid withdrawal symptoms, including respiratory depression, anxiety, and abdominal pain. This may occur even in individuals who are no longer actively using opioids but have residual dependency.
Opioid withdrawal or opioid addiction history must be ruled out before treatment initiation. This is especially important for patients being treated for alcohol and opioid addiction or undergoing nicotine replacement therapy, as bupropion inhibits the reward cycle reinforcement.
Likewise, alcohol dependence or active alcohol use may worsen adverse reactions, particularly joint pain, abdominal pain, and liver-related complications in those with severe hepatic impairment.

Common Side Effects and Adverse Reactions
When bupropion naltrexone and modafinil are taken together, the likelihood of experiencing adverse reactions increases due to their overlapping effects on the central nervous system and metabolism. While not everyone will experience problems, some symptoms are more commonly reported—especially during the early weeks of combined therapy or following a dosage adjustment.
The most frequently observed side effects in individuals using both medications include:
- Headache
- Nausea
- Abdominal pain
- Anxiety or restlessness
- Insomnia or disrupted sleep patterns
- Joint pain
These effects may occur independently or be amplified when the medications are used together. In many cases, they are mild and temporary—resolving as the body adapts to the medications. However, in some individuals, these reactions may occur persistently and require intervention. This could involve a dose reduction, a slower dosage increase, or even discontinuation of one of the drugs.
Importantly, some side effects—such as abdominal pain, joint pain, and chest pain—can mimic symptoms of more serious complications like cardiovascular events or hypertensive reactions. These should not be ignored and must be evaluated promptly by a healthcare provider.
In certain patients, side effects may emerge as part of broader psychiatric disorders, particularly if there’s a history of bipolar disorder, obsessive-compulsive disorder, or anxiety. These individuals may be more sensitive to changes in neurotransmitter levels caused by either drug.
At the biochemical level, the active metabolite of bupropion—known as hydroxybupropion—is largely responsible for the medication’s therapeutic and side-effect profiles. This metabolite is formed via the liver enzyme CYP2B6. However, modafinil is known to modulate cytochrome P450 activity, including CYP2B6, potentially interfering with the metabolic processing of bupropion, according to a study published on the NIH website.
This interference can lead to altered systemic exposure, resulting in statistically significant differences in the blood levels of bupropion and its metabolite. In real-world terms, this means that some patients may absorb too much of the active compounds, which could intensify side effects like high blood pressure, insomnia, or the risk of seizures.
Additionally, combining modafinil with other drugs that rely on the same metabolic enzymes—such as tricyclic antidepressants, antipsychotics, or systemic corticosteroids—could further complicate the body’s ability to safely process these substances. This increases the importance of reviewing all medications and supplements a patient is taking before starting combined therapy.
For those already on treatment, healthcare providers should monitor patients regularly for emerging symptoms and educate them on what to watch for—especially any signs of worsening abdominal pain, sustained anxiety, or chest pain. Early intervention can help prevent more serious complications and ensure the therapeutic effects of the treatment are not overshadowed by avoidable side effects.
Special Considerations for Dosing
Due to the increased risk of respiratory depression, abdominal pain, or seizure activity, gradual titration is essential. Physicians may recommend a slower dosage increase for Contrave when used with modafinil, especially in obese adults with body mass index thresholds above 30.
Also, taking Contrave with high-fat meals increases the rate of absorption, which may further complicate the interaction profile. A reduced-calorie diet is still recommended during contrave treatment, and patients should avoid fatty meals to minimize adverse reactions.
Smoking Cessation and Additional Therapeutic Use
Bupropion naltrexone is sometimes explored for smoking cessation, particularly for those with overlapping food cravings and nicotine dependence. Since modafinil also has off-label potential in attention and addiction disorders, the interaction profile may be complicated by therapeutic benefits across multiple domains, including neuropathic pain and attention-related issues.
Nevertheless, care must be taken not to assume enhanced efficacy simply because both medications affect mood, energy, or appetite. The combined therapeutic effects may be unpredictable and depend heavily on individual risk factors and metabolic rates.
Guidelines for Patients and Physicians
Patients considering or currently taking both Contrave and modafinil should:
- Disclose all current medications, including supplements and systemic corticosteroids or tricyclic antidepressants.
- Alert their doctor to any history of opioid addiction, alcohol dependence, or psychiatric disorders.
- Report side effects such as abdominal pain, joint pain, chest pain, or mood changes immediately.
- Understand that dose adjustment may be necessary at several stages of treatment.
- Avoid self-adjusting doses or substituting other drugs without physician oversight.
Frequently Asked Questions (FAQ)
Understanding how medications interact is essential for safety and treatment success.
Below are some of the most common questions about taking bupropion naltrexone (Contrave) and modafinil, as well as related drug combinations. Always consult your healthcare provider before starting or combining any medications.
1. Can you take modafinil and bupropion together?
Modafinil and bupropion may be taken together in some cases, but the combination should be approached with caution. Both drugs affect dopamine levels in the brain, which may increase the risk of seizures, especially in patients with a history of neurological conditions.
Additionally, modafinil may interfere with the metabolism of bupropion, potentially raising blood levels and the likelihood of adverse reactions. Doctors may recommend a dose adjustment or additional monitoring if these drugs are prescribed together.
2. What medications to avoid with Contrave?
Several medications should be avoided when taking Contrave due to potentially serious drug interactions. These include opiate agonists (such as codeine, hydrocodone, or morphine), as naltrexone may cause sudden opioid withdrawal symptoms. Monoamine oxidase inhibitors (MAOIs), used to treat depression, are also contraindicated, as combining them with bupropion therapy can lead to severe high blood pressure or serotonin syndrome. Other antidepressants can also cause adverse effects. Our recent article on taking Contrave and Paxil drug interactions explores this topic in depth.
Patients should also use caution with tricyclic antidepressants, antipsychotics, and other medications that lower the seizure threshold.
3. What drugs should not be taken with modafinil?
Medications that interact with the liver enzyme system—particularly CYP3A4 and CYP2B6—can be problematic when used with modafinil. This includes tricyclic antidepressants, hormonal contraceptives, and systemic corticosteroids, which may become less effective or increase the risk of side effects.
Additionally, modafinil can interfere with other drugs used to treat mental health conditions, increasing the risk of serotonin syndrome or cardiovascular effects. Patients with psychiatric disorders or those on complex regimens should be closely supervised if modafinil is introduced.
4. Can you take phentermine and Contrave at the same time?
Phentermine and Contrave are sometimes used together for weight loss, but this combination is not FDA-approved and carries certain risks. Both drugs can raise blood pressure and heart rate, increasing the chance of hypertensive reactions, chest pain, or abdominal pain in sensitive individuals.
There is also a concern about overstimulation of the central nervous system, which may heighten anxiety or the risk of seizures. If a physician considers combining them, they will likely recommend close monitoring and start with low doses to reduce potential harm.
Summary
Although combining modafinil and Contrave may seem appealing for patients aiming to lose weight while staying mentally alert, the combination introduces a web of possible drug interactions and side effects. The risk of seizures, increased blood pressure, serotonin syndrome, and opioid withdrawal symptoms makes it crucial for providers to monitor closely and educate patients thoroughly.
Physicians should review each patient’s history for opiate agonists, cardiovascular issues, and mental health conditions before initiating bupropion or adding modafinil. With tailored oversight, some patients may experience meaningful therapeutic effects, but safety must remain the top priority.
References