GLP-1 Drugs: Benefits, Mental Health Impacts, & Accessibility
Dr. Matthew Olesiak, MD, is the Chief Medical Director at SANESolution, a renowned wellness technology company dedicated to providing evidence-based solutions for optimal living. Dr. Olesiak earned his medical degree from the prestigious Jagiellonian University Medical College in Kraków, Poland, where he developed a strong foundation in medicine.
Introduction
GLP-1 medications, short for glucagon-like peptide-1 receptor agonists, are transforming the landscape of weight loss and health management. Originally developed to treat type 2 diabetes mellitus, these medications—such as Ozempic, Saxenda and Wegovy —have become widely recognized for their ability to promote significant weight loss. Their growing popularity stems from their dual role: aiding in weight management while improving blood sugar control, making them a powerful option for compatible individuals struggling with obesity or related conditions.
What makes GLP-1 drugs unique is their mechanism of action. These medications mimic a naturally occurring hormone, GLP-1, that plays a key role in appetite regulation and glucose metabolism. By slowing digestion, enhancing feelings of fullness, and stabilizing blood sugar levels, GLP-1 drugs help reduce calorie intake and foster sustainable weight loss.
In this article, we’ll explore GLP-1 drugs benefits, as well as their long-term safety and efficacy, their potential impacts on mental health, and challenges related to accessibility. Additionally, we’ll discuss how these medications can be integrated into a holistic approach to health, emphasizing the importance of lifestyle changes for sustained success.
Key Takeaways
- Beneficial for Weight Loss: GLP-1 drugs like Wegovy and Ozempic support significant weight loss but require consistent use and adherence to lifestyle changes for long-term success.
- Mental Health Impacts: The psychological effects vary—some users report boosted self-esteem, while others may experience challenges like anxiety or mood shifts.
- Accessibility Challenges: High costs and limited insurance coverage pose barriers, making these drugs less accessible for many people.
Long-Term Safety and Efficacy
Overview of Clinical Trials
GLP-1 receptor agonists have been extensively studied in clinical trials, initially for managing type 2 diabetes and more recently for weight loss. Trials such as the STEP program, which evaluated semaglutide (Wegovy), have shown promising results. Over 68 weeks, participants taking semaglutide experienced an average weight loss of 15% of their body weight compared to 2.4% in the placebo group. Similarly, trials for liraglutide (Saxenda) demonstrated weight loss of approximately 5–10% over a year when combined with lifestyle interventions.
These results highlight the efficacy of GLP-1 drugs for significant, sustained weight loss. However, adherence is critical, as discontinuation often leads to weight regain. Long-term studies are ongoing to evaluate how these medications perform over several years, but early findings indicate that continued use is essential for maintaining results.
Sustainability of Weight Loss
While GLP-1 therapy offers significant weight loss, sustainability remains a key challenge. Research shows that once the medication is stopped, many users experience weight regain. This occurs because GLP-1 drugs address hormonal imbalances contributing to overeating but do not permanently alter underlying physiological mechanisms.
Strategies to mitigate weight regain include:
- Lifestyle Modifications: Incorporating regular physical activity and balanced nutrition helps maintain results after stopping the medication.
- Behavioral Support: Working with healthcare providers or therapists to develop long-term strategies for managing eating behaviors and stress can enhance success.
- Gradual Tapering: Slowly reducing the dose under medical supervision may help some individuals transition off the drug with minimal rebound effects.
Emerging Risks
While generally well-tolerated, GLP-1 drugs are associated with potential risks, especially with prolonged use.
Common side effects include nausea, vomiting, and diarrhea, which tend to improve over time. However, more serious concerns have emerged in clinical and observational studies:
- Gallbladder Issues: Rapid weight loss linked to GLP-1 drugs increases the risk of gallstone formation and gallbladder disease. Symptoms include abdominal pain, nausea, and fever, and in some cases, surgical intervention may be required.
- Pancreatitis: Though rare, GLP-1 drugs have been associated with cases of acute pancreatitis, an inflammation of the pancreas. Symptoms include severe abdominal pain, nausea, and vomiting. While the risk is low, individuals with a history of pancreatitis may need alternative treatments.
- Thyroid Tumors: In animal studies, GLP-1 drugs have been linked to an increased risk of medullary thyroid cancer. Although this finding has not been confirmed in humans, healthcare providers typically avoid prescribing these medications to individuals with a family history of thyroid cancer or certain genetic conditions.
- Kidney Injury: Side effects such as nausea and vomiting can lead to acute kidney injury due to volume contraction. It is important for healthcare providers to counsel patients on managing these side effects to prevent kidney-related complications.
To minimize risks, regular monitoring by a healthcare provider is essential. This includes periodic assessments of gallbladder health, pancreatic function, and thyroid markers where appropriate.
The long-term safety and efficacy of GLP-1 drugs have been seen in clinical trials, making them a valuable tool for weight loss. However, sustained results require ongoing use or comprehensive lifestyle changes, and certain risks must be carefully managed.
By understanding these factors, individuals and healthcare providers can make informed decisions about incorporating GLP-1 medications into a long-term health strategy.
Mental Health Impacts
Positive Effects
The psychological benefits of GLP-1 medications often stem from the physical transformations they facilitate. Many users report improved self-esteem and emotional well-being as they experience weight loss and related health improvements. Shedding excess weight can alleviate the emotional burdens associated with obesity, such as social stigma, reduced mobility, and health-related anxieties.
Moreover, GLP-1 drugs may indirectly improve mental health by addressing conditions linked to obesity, such as sleep apnea, type 2 diabetes, improved blood glucose levels, and joint pain. For instance, better sleep quality and reduced fatigue can enhance overall mood and cognitive function, contributing to a sense of vitality and empowerment.
However, it’s important to note that these benefits are not universal. The degree of psychological improvement depends on individual factors, including personal goals, support systems, and pre-existing mental health conditions.
Potential Risks, including Kidney Disease
While the physical benefits of GLP-1 medications are well-documented, the rapid weight changes they induce can present mental health challenges. Significant or swift weight loss may disrupt body image, especially in individuals with pre-existing insecurities about their appearance. Some users report feeling disconnected from their changing bodies, which can lead to anxiety or depression.
Additionally, the intense focus on weight loss during treatment can exacerbate emotional pressure to maintain results, potentially triggering stress or feelings of failure if progress slows or weight is regained. These risks highlight the importance of psychological support during and after treatment.
For individuals prone to mood disorders, such as anxiety or depression, it’s critical to monitor for any mental health shifts during GLP-1 use. While no direct causal relationship has been established, some anecdotal reports suggest that changes in appetite and weight regulation may impact emotional stability.
Eating Disorders Intersection
The use of GLP-1 medications in individuals with a history of disordered eating requires careful consideration. These drugs significantly alter appetite and food intake, which could potentially exacerbate unhealthy eating patterns. For instance, their appetite-suppressing effects may encourage restrictive behaviors in individuals prone to anorexia or lead to a reliance on the medication for control over food intake.
Conversely, individuals with binge eating disorder (BED) may benefit from GLP-1 drugs, as they help regulate appetite and reduce the frequency of overeating episodes. Clinical trials have demonstrated that GLP-1 medications can significantly improve control over bingeing behaviors, particularly in individuals with concurrent obesity.
Healthcare providers must thoroughly evaluate a patient’s history before prescribing GLP-1 drugs to those with eating disorders. Ongoing monitoring is essential to ensure that the medication supports recovery rather than hindering it. Incorporating behavioral therapy alongside medication can further safeguard mental health and promote a balanced approach to weight loss.
GLP-1 medications offer notable mental health benefits for many individuals, including improved self-esteem and emotional well-being. However, potential risks, such as body image concerns and the psychological challenges of rapid weight loss, should not be overlooked.
For individuals with a history of eating disorders, the use of these medications must be approached cautiously and with comprehensive support. Ultimately, a personalized and holistic treatment plan can help ensure that mental health and physical health goals are aligned.
Accessibility and Economic Considerations
Cost Comparison
One of the major barriers to GLP-1 medications is their high cost, which can make them inaccessible to many individuals. On average, the monthly cost for medications like Wegovy, Ozempic, or Saxenda ranges from $800 to $1,500 without insurance. Generic alternatives are not yet available for most GLP-1 drugs, keeping prices relatively high compared to other weight loss treatments.
For individuals managing multiple health conditions, these costs can add up quickly. Although some drug manufacturers offer savings programs or assistance for eligible patients, many people fall outside the income requirements or coverage limits for these programs.
In contrast, lifestyle interventions such as dietary counseling and exercise programs may appear more cost-effective in the short term. However, they often lack the immediate and sustained results seen with GLP-1 drugs, complicating the cost-benefit analysis for those seeking significant weight loss.
Insurance Challenges
Insurance coverage for GLP-1 medications is inconsistent and varies widely by provider and plan. Some insurers classify these drugs as “lifestyle” treatments rather than essential therapies, limiting reimbursement options. Even when covered, plans often impose strict requirements, such as prior authorization or evidence of a BMI above 30 (or 27 with comorbidities).
Patients frequently report delays in obtaining coverage or having to appeal denials, creating additional stress and financial burdens. For those with high-deductible plans, out-of-pocket expenses may still be prohibitively high, even with partial coverage.
Medicare, which serves a significant portion of older adults, does not currently cover GLP-1 medications for weight loss, though it may cover them for type 2 diabetes management. This leaves many patients paying full price unless alternative funding sources, such as employer-sponsored wellness programs, are available.
Economic Impact
Despite their upfront costs, GLP-1 medications have the potential to reduce healthcare spending over the long term. Obesity-related conditions, such as type 2 diabetes, hypertension, heart disease, and kidney disease, are major drivers of healthcare costs in the U.S. Treating these conditions often requires ongoing management through medications, hospitalizations, and procedures, all of which add significant financial strain to the healthcare system.
Studies have shown that GLP-1 medications not only promote weight loss but also improve metabolic markers like blood sugar levels and cholesterol. By reducing the prevalence and severity of obesity-related diseases, including kidney disease, these medications could lead to substantial savings for both patients and healthcare systems. For example, one analysis estimated that for every 10% reduction in body weight, annual healthcare costs could decrease by up to $5,000 per person.
Additionally, improved productivity and reduced absenteeism in the workplace may yield further economic benefits, particularly for individuals whose weight-related health issues previously limited their daily functioning.
The high cost of GLP-1 medications and inconsistent insurance coverage remain significant barriers to accessibility. However, the potential for long-term healthcare savings through reduced obesity-related conditions highlights their value beyond immediate weight loss.
Addressing these challenges will require policy changes, increased competition in the pharmaceutical market, and greater recognition of obesity as a medical condition deserving comprehensive treatment.
Personalized Medicine and Diverse Populations
Tailoring Treatments
The future of GLP-1 medications lies in personalized medicine, where treatments are tailored to an individual’s unique genetic, metabolic, and microbiome profile. Early research suggests that genetic variations may influence how effectively someone responds to GLP-1 drugs. For example, genes involved in appetite regulation and glucose metabolism could determine the degree of weight loss or improvement in blood sugar control.
Additionally, the gut microbiome—the collection of bacteria and microorganisms in the digestive tract—plays a pivotal role in how the body processes food and responds to medications. Studies are beginning to explore whether specific microbiome compositions make some individuals more likely to benefit from GLP-1 drugs.
While this field is still emerging, future advancements could allow healthcare providers to use microbiome testing or genetic analysis to predict a patient’s response to treatment, improving outcomes and reducing trial-and-error prescribing.
Population-Specific Effectiveness
GLP-1 drugs are not one-size-fits-all; their efficacy varies across different demographics. For older adults, these medications can be particularly beneficial in addressing age-related weight gain and managing comorbidities such as type 2 diabetes. However, older individuals may also face a higher risk of certain side effects, such as gastrointestinal distress or gallbladder issues, requiring careful monitoring by healthcare providers.
In people with type 2 diabetes, GLP-1 drugs offer dual benefits by improving glycemic control and promoting weight loss. These outcomes can significantly reduce the risk of diabetes-related complications, such as cardiovascular disease and kidney damage.
However, dosing and efficacy may vary depending on the severity of the individual’s diabetes and their baseline weight. Insurance plans often require evidence of a body mass index (BMI) above 30 or 27 with comorbidities for coverage of these medications.
Research also suggests that GLP-1 medications may work differently across ethnic groups due to genetic and metabolic differences. For instance, certain populations may metabolize the drug more slowly, leading to prolonged effects or increased side effects. Unfortunately, clinical trials often lack diversity, making it challenging to fully understand how these medications perform in underrepresented groups.
Personalized medicine is poised to revolutionize the use of GLP-1 drugs, enabling tailored treatments based on genetic and microbiome profiles. Meanwhile, understanding how these medications perform in various populations is essential for optimizing their use.
By addressing these factors, healthcare providers can ensure that GLP-1 therapies are effective, safe, and equitable for all patients.
Behavioral and Lifestyle Integration
Pairing Medications with Lifestyle Changes
GLP-1 medications are primarily injectable medications used to manage weight and blood sugar levels. These drugs are most effective when combined with healthy lifestyle changes.
While these drugs significantly aid weight loss by regulating appetite and blood sugar, sustainable results require adopting supportive habits.
- Exercise: Regular physical activity enhances the benefits of GLP-1 drugs. Cardiovascular exercises like walking, swimming, or cycling improve metabolism and cardiovascular health, while strength training helps maintain muscle mass during weight loss. Experts recommend at least 150 minutes of moderate activity per week, tailored to an individual’s fitness level.
- Nutrition: A balanced diet is key to maximizing the effectiveness of GLP-1 medications. Prioritize nutrient-dense foods like lean proteins, legumes, and vegetables, which support satiety and prevent nutrient deficiencies. Avoid relying solely on appetite suppression and focus on mindful eating habits.
- Behavioral Therapy: For many individuals, weight struggles are tied to emotional or habitual eating. Behavioral therapy or counseling can help identify triggers, establish healthier coping mechanisms, and create sustainable eating patterns that align with the medication’s effects.
Maintaining Results Post-Medication
One of the biggest challenges with GLP-1 drugs is maintaining weight loss after discontinuation. Without the appetite-regulating effects of the medication, the risk of weight regain increases significantly. To counter this, it’s essential to build habits that support long-term weight management:
- Consistent Physical Activity: Develop an exercise routine that becomes a regular part of daily life, even after stopping the medication. Consistency is more important than intensity for long-term adherence.
- Nutritional Awareness: Learn portion control, meal planning, and mindful eating techniques to prevent overeating after medication withdrawal.
- Behavioral Support: Continue working with a therapist, dietitian, or support group to navigate challenges and maintain accountability.
Gradual tapering of the medication under medical supervision may also help ease the transition and reduce the likelihood of rapid weight regain.
Practical Tips
To get the most out of GLP-1 medications, consider these actionable strategies:
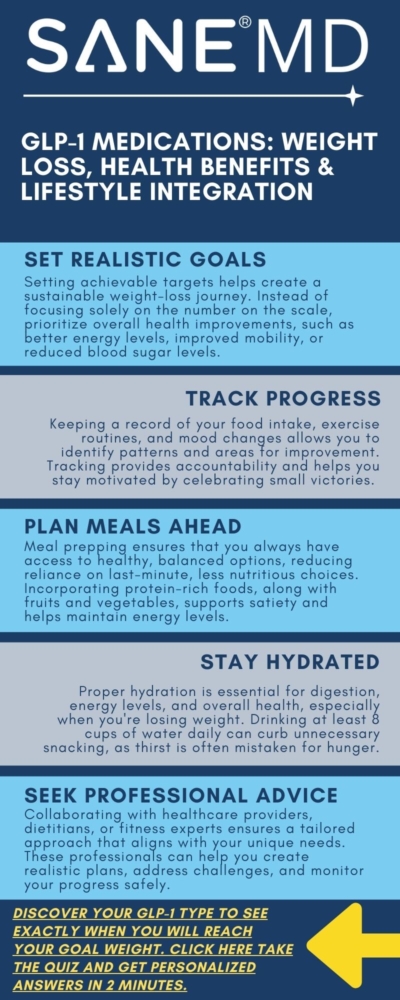
- Set Realistic Goals: While GLP-1 drugs can produce significant weight loss, it’s important to set achievable targets and avoid unhealthy expectations. Focus on overall health improvements rather than just numbers on the scale.
- Track Progress: Use a journal or app to monitor your food intake, exercise, and any changes in mood or energy levels. Tracking helps identify patterns and areas for improvement.
- Plan Meals Ahead: Preparing meals in advance reduces the temptation to opt for less healthy options. Incorporate protein-rich snacks to sustain energy levels and support satiety.
- Stay Hydrated: Proper hydration supports digestion, energy levels, and overall well-being, especially during weight loss. Aim for at least 8 cups of water daily.
- Seek Professional Guidance: Work with a healthcare provider, dietitian, or fitness trainer to develop a personalized plan that complements the effects of the medication.
GLP-1 medications work best as part of a comprehensive approach to health, including exercise, balanced nutrition, and behavioral support. Building sustainable habits not only enhances the drug’s effects but also helps maintain weight loss after discontinuation.
By integrating these practical strategies, individuals can achieve lasting results and improve their overall well-being.
Frequently Asked Questions (FAQs)
GLP-1 medications are becoming increasingly popular for weight loss and health management, but their unique mechanisms and potential impacts often raise questions.
Below, we address some of the most common concerns to help individuals make informed decisions about these medications.
1. What are GLP-1 drugs, and how do they work?
GLP-1 drugs, also known as GLP-1 agonists, mimic a naturally occurring hormone called glucagon-like peptide-1, which is involved in appetite and blood sugar regulation. These medications slow down digestion and increase feelings of fullness, helping individuals eat less and lose weight.
Additionally, they improve blood sugar control, making them particularly effective for people with type 2 diabetes.
2. Are GLP-1 drugs safe for long-term use?
Long-term use is generally considered safe for most people, as supported by clinical trials and post-market studies. However, some risks, such as gallbladder issues, pancreatitis, or gastrointestinal discomfort, have been reported.
Regular medical monitoring is crucial to ensure safety, especially for individuals with pre-existing conditions. Discuss any concerns with your healthcare provider before starting treatment.
3. What is the average weight loss with GLP-1 medications?
Weight loss results vary, but clinical trials show that individuals using GLP-1 drugs like Wegovy or Saxenda typically lose 10–15% of their initial body weight over several months.
These outcomes depend on consistent use and incorporating healthy lifestyle changes, such as regular exercise and a balanced diet.
4. Do GLP-1 drugs have any mental health side effects?
Many users experience improved mental health as a result of weight loss and better overall health. However, some report mood changes, anxiety, or depression while using GLP-1 medications.
While these side effects are not common, it’s essential to monitor your mental health and discuss any changes with your healthcare provider.
5. Are GLP-1 drugs covered by insurance?
Insurance coverage for GLP-1 medications varies widely. While some plans cover these drugs, they often require prior authorization or proof of medical necessity, such as a BMI above a specific threshold. Out-of-pocket costs can be high without coverage.
Patients should review their insurance plan details or consult with their provider to understand their options.
Conclusion
GLP-1 medications offer a promising approach to weight loss and health management by combining appetite regulation with improvements in blood sugar control. Their benefits extend beyond weight loss, enhancing physical and mental well-being for many users.
However, these drugs come with challenges, including potential side effects, accessibility barriers, and the need for lifestyle integration.
By working closely with healthcare providers, individuals can navigate these challenges and develop a personalized plan that aligns with their health goals.
References
- Clinical trials and studies: STEP program, SCALE study.
- Reputable health organizations: American Diabetes Association, National Institutes of Health.
- Drug-specific information: Manufacturer websites (e.g., Novo Nordisk).