GERD management and treatment involve a multi-faceted approach. It’s not just about controlling the symptoms; it’s also about healing the inflammation or irritation of the esophagus (esophagitis) and preventing recurring complications.
In this informative SANE MD blog post, we’ll explore the various symptoms and causes of GERD before delving into its management and treatment options to help you better understand this complex chronic acid reflux disease.
Want to learn even more about GERD? Check out our How to Cure GERD Permanently? A Comprehensive Guide and if you have trouble with asthma, head over to our A Guide to Asthma Medications and Treatments: What You Need to Know post!
Key Takeaways
- GERD, or Gastroesophageal Reflux Disease, is a chronic condition caused by stomach acid reflux into the esophagus, leading to symptoms such as heartburn, chest pain, and regurgitation.
- Lifestyle modifications such as weight loss, avoiding foods that trigger acid reflux, and lifting the head of the bed can help manage GERD symptoms. Medications such as antacids, proton pump inhibitors, and H2 blockers may also be prescribed.
- In severe cases, surgery may be necessary to treat GERD. Working closely with a healthcare provider is essential to determine the best treatment for managing and treating GERD.
What Is Gastroesophageal Reflux Disease?
GERD stands for gastroesophageal reflux disease, a medical condition that occurs when stomach contents flow back into the esophagus, causing frequent episodes of acid reflux. This happens due to the lower esophageal sphincter, a ring of muscle at the bottom of the esophagus, not closing correctly or opening at inappropriate times.
During normal digestion, the Lower Esophageal Sphincter (LES) opens up to allow food into the stomach. It then promptly closes to prevent the backward flow of food and acidic stomach juices into the esophagus. However, when the LES is weak or relaxes when it shouldn’t, it allows the stomach’s contents to flow back into the esophagus, leading to a condition called acid reflux or Gastroesophageal Reflux (GER).
Acid reflux is considered chronic when it occurs at least twice a week for several weeks. While diet and other factors can cause temporary acid reflux, GERD is a chronic condition that requires medical attention.
It is important to seek medical help for GERD because, if left untreated, repeated gastric acid secretion can damage the esophagus and lead to severe complications.
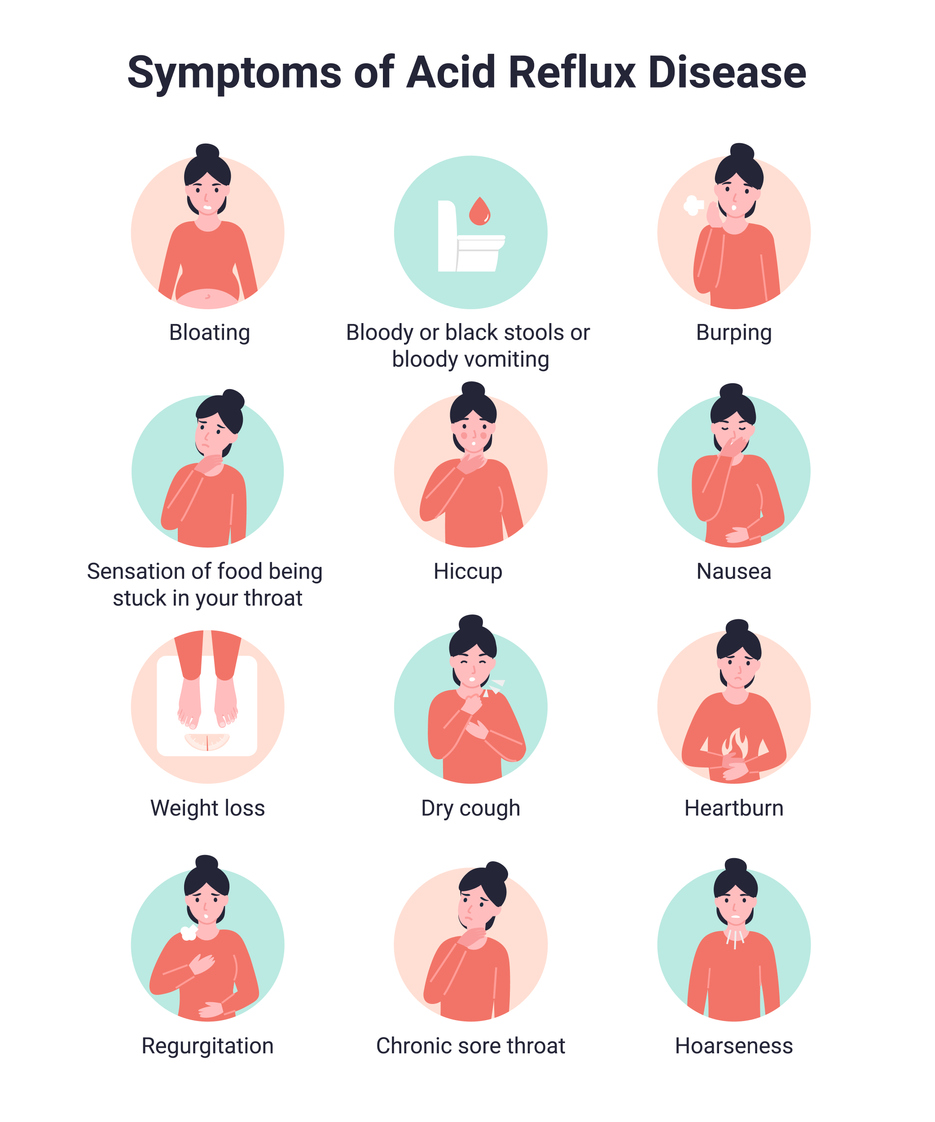
Infographic Text
Symptoms of Acid Reflux Disease
Bloating, bloody or black stools or bloody vomiting, burping, sensation of food being stuck in your throat, hiccup, nausea, weight loss, dry cough, heartburn, regurgitation, chronic sore throat, hoarseness.
End Infographic Text
Prevalence of Acid Reflux and GERD
Occasional acid reflux and gastroesophageal reflux disease (GERD) are common ailments. In the United States, GERD affects approximately 20% of adults and 10% of children (1), and this is not a minor health issue.
The National Institute of Diabetes and Digestive and Kidney Diseases reports that GERD was responsible for 4.7 million hospitalizations and 1,653 deaths in 2010 (2).
GERD Symptoms
Typical GERD symptoms include:
- Heartburn, a burning sensation in the chest that can sometimes spread to the throat
- Acid indigestion (dyspepsia), a range of gastrointestinal symptoms that co-occur, such as abdominal discomfort after eating, pain in the upper abdomen, or the feeling of fullness after eating just a little bit of food.
- Chest pain
- Nausea
- Belching
- Feeling like your stomach is bloated
- Regurgitation of swallowed food
- A sour taste in your mouth
- Bad breath
- Wheezing
- Sore throat
- Chronic coughing
- Difficulty swallowing
- The sensation of a lump in your throat
- Frequent throat clearing
- Dry cough
- Hoarseness

It should be noted that the most common symptoms of acid reflux/GERD are heartburn and acid indigestion.
However, if you have laryngopharyngeal reflux (LPR) or silent reflux, you may not experience heartburn or acid indigestion. Instead, your symptoms may be throat-related, such as breathing difficulties, hoarseness, chronic cough, the sensation of something stuck in your throat, frequent throat clearing, and postnatal drip.
Acid Reflux and GERD Risk Factors
The following factors can weaken your LES, leading to occasional acid reflux and, in certain circumstances, GERD:
Overweight and Obesity
The World Health Organization (WHO) defines overweight and obesity as “abnormal or excessive fat accumulation that presents a risk to health.” (3)
One of these health risks is GERD.
According to the American Society for Gastrointestinal Endoscopy, obesity is the primary cause of frequent acid reflux and heartburn (4).
But you don’t have to be overweight to develop GERD. Research suggests that any weight gain increases your risk of developing this gastrointestinal disorder or exacerbates the symptoms even if you are of average weight (5). Amazingly, it’s not the number on the scale that’s important for GERD; it’s the weight distribution. If your weight gain comes from fat accumulation in your abdomen, you’re at risk of acid reflux and GERD.
You see, abdominal obesity is a significant risk factor in developing GERD because it puts pressure on the abdomen, which compromises the integrity of the LES, making it open at inappropriate times and decreasing the pressure needed to keep it firmly closed when necessary (6).
Hiatal Hernia
A hiatal hernia occurs when the upper part of the stomach protrudes into the chest area, which causes the stomach to press against the lower opening of the esophagus. This can result in stomach acid traveling upward, leading to acid reflux (7).
A hiatal hernia increases the chances of developing GERD (8); almost half of people diagnosed with GERD also have a hiatal hernia.
People with larger hiatal hernias are more likely to experience severe GERD symptoms.
Pregnancy
Acid reflux is common during pregnancy and can result from several causes.
The increased pressure and volume in the abdomen can push, stretch, and weaken the muscles in your diaphragm that support your lower esophageal sphincter (LES). Additionally, pregnancy hormones such as relaxin can encourage your LES to relax, making it easier for stomach acid to flow back into your esophagus. High levels of estrogen and progesterone during pregnancy may also contribute to LES relaxation.
In most cases, acid reflux subsides after delivery without causing any complications.

Gastroparesis
Gastroparesis is a medical condition that affects the natural movement of the muscles in the stomach. Strong muscular contractions push food through the digestive tract in a healthy stomach. However, in the case of gastroparesis, the stomach’s motility is slowed down or completely stopped, which hinders the proper emptying of the stomach.
Studies (10) have linked gastroparesis to gastroesophageal reflux disease (GERD). Because of the delayed stomach emptying due to gastroparesis, food can remain in the stomach for an extended period, significantly increasing the risk of developing acid reflux and GERD.
Connective Tissue Disorder
Connective tissue disorder is a medical condition that causes damage to collagen and elastin, which are vital proteins in the body that connect tissues, bones, and organs. Collagen is present in tendons, ligaments, cartilage, and blood vessels, while elastin is the critical component of ligaments and skin, giving them stretchy properties.
In individuals with a connective tissue disorder, the collagen and elastin undergo inflammation, damaging the body parts they connect. Since the LES contains a significant amount of connective tissue, it is particularly susceptible to this damage.
Examples of connective tissue disorders include rheumatoid arthritis, lupus, Marfan syndrome, and scleroderma.
Medications
Specific medications have been shown to loosen the LES, increasing the risk of acid reflux. These medications include:
- Certain high blood pressure medications, like calcium channel blockers
- Nonsteroidal anti-inflammatory drugs (NSAIDs), like aspirin and ibuprofen
- Benzodiazepines (sedatives), like Valium and Xanax
- Hormone replacement therapy for menopause
- Tricycle antidepressants for depression and pain
Lifestyle Factors
Smoking
Smoking is a terrible habit that negatively affects most bodily functions, including the gastrointestinal tract. For example, tobacco smoke can cause relaxation of the lower esophageal sphincter (LES), whether you are smoking yourself or just exposed to second-hand smoke.
Smoking also triggers coughing, which can further weaken your LES. Over time, smoking and chronic coughing can also cause your diaphragm muscles to weaken, potentially leading to a hiatal hernia.
Additionally, smoking can slow down digestion and increase stomach acid production.
Dietary Habits
While foods and drinks may not cause acid reflux, they can contribute to it. Consuming spicy foods, chocolate, coffee, alcohol, garlic, citrus fruits, onions, tomatoes, and mint in higher doses can relax your LES. On the other hand, fatty foods increase stomach acid and take longer to digest, giving acid more time to escape the stomach.
In addition, eating large meals or lying down immediately after eating can promote acid reflux and, if it occurs frequently, can lead to GERD.
Exercise
Physical exercise is generally considered healthy but can aggravate acid reflux, especially during intense exercise (11).
Specific exercises can reduce blood flow to your gastrointestinal area, which can cause gastric fluids to accumulate in a specific area, resulting in inflammation and irritation. Restrictive body positions during exercise can also put pressure on your abdominal and chest area, leading to symptoms.
Some movements that can trigger symptoms include hanging upside down and bending for extended periods.
During high-impact exercise, gulping air may relax the lower esophageal sphincter, forcing acid into the esophagus.
High-intensity exercises that may exacerbate acid reflux symptoms include:
- Running
- Cycling
- Sprinting
- Jumping rope
- Weight lifting
Eating before a workout can also increase the risk of exercise-induced acid reflux.

GERD Complications
Stomach acid is a potent substance designed to break down the food you consume for digestion. The inner lining of your stomach is built tough to protect it from its acid. However, your esophagus, throat, larynx, mouth, and teeth lack this protection. Severe acid reflux can affect your entire oral cavity, even damaging tooth enamel. It can also promote vocal cord growths or cause acid to be drawn into the lung.
GERD complications can include:
- Esophagitis. Esophagitis is inflammation in the lining of the esophagus that can cause chronic pain, ulcers, scarring, and even a precancerous condition called Barrett’s esophagus.
- Barrett’s esophagus. Barrett’s esophagus is a condition where the tissues lining the esophagus change to resemble those of the intestine due to prolonged exposure to acid and inflammation. This condition is a risk factor for esophageal cancer.
- Esophageal stricture. In response to chronic inflammation and injury, your esophagus may produce scar tissue as a protective measure. The scar tissue may result in a condition called esophageal stricture, which can cause your esophagus to narrow. As a result, swallowing can become difficult, making it challenging to eat and drink.

GERD Management
The management of gastroesophageal reflux involves reducing reflux and minimizing damage to the esophageal lining. This can usually be accomplished with medicines, lifestyle changes, and surgical treatment.
Medication Regimen to Treat GERD
To treat GERD, your doctor may recommend an over-the-counter or prescription medication that may include one or more of the following:
Antacids
There are drugs available that can help neutralize acid in the esophagus and stomach, which can stop heartburn. Nonprescription antacids can provide temporary or partial relief for many people. Some people find that combining an antacid with a foaming agent helps them. These compounds are believed to create a foam barrier on top of the stomach, preventing acid reflux.
However, long-term use of antacids can cause side effects such as diarrhea, a change in how the body metabolizes metabolism, and a buildup of magnesium. Too much magnesium can be severe for people who have kidney disease. Therefore, if you need antacids for over two weeks, you must talk to your doctor.
Proton pump inhibitors (PPIs)
Proton pump inhibitors (PPIs) are a type of medication that works by blocking and reducing the production of stomach acid, helping to heal any damaged esophageal tissue and prevent heartburn – one of the primary symptoms of GERD.
It typically takes PPIs four to twelve weeks to gradually decrease stomach acid. This timeframe allows for proper healing of the esophageal tissue. Unlike H2 receptor blockers, which can reduce stomach acid within an hour, PPIs may take longer to ease your symptoms. Nevertheless, symptom relief from PPIs lasts longer. Therefore, PPI medications are most appropriate for those with GERD.
Popular PPI brand names include Nexium, Prevacid, and Prilosec.
H2 receptor blockers
For chronic reflux and heartburn, the doctor may recommend H2 receptor blockers to reduce acid in the stomach.
How do H2 blockers work?
Histamine, a chemical in our body, prompts cells in the stomach lining to generate hydrochloric acid. Excessive production of this acid can lead to GERD and other painful conditions.
H2 blockers bind to the histamine receptors in the stomach, thereby reducing the amount of acid the stomach lining secretes. This helps relieve the symptoms caused by excessive stomach acid.
The effects of this medication can usually be felt within 60 minutes (12) and can last for 4 to 10 hours.
Lifestyle Changes
Acid reflux/GERD can often be managed with lifestyle changes.
- Avoid eating large portions. To reduce acid production and minimize reflux, consuming smaller portions of food is recommended during mealtime.
- Do not eat before bedtime. Eating your last meal at least 2-3 hours before bedtime allows digestion and stomach emptying, reducing acid reflux.
- Eat slowly and chew food well. Chewing food thoroughly can help prevent the risk of choking and swallowing air while also promoting the production of saliva, which neutralizes stomach acid because it is alkaline. Health experts advise chewing each bite of food between 10 to 20 times for best results.
- Elevate your head while reclining. Elevating the head of your bed with 6-inch blocks or using a specially designed wedge while sleeping can help reduce the amount of stomach contents that flow back into your esophagus due to the force of gravity. Using pillows to prop yourself up is not recommended, as it can increase pressure on your stomach.
- Wear comfortable, loose clothing. Clothing compressing the waist can increase the risk of acid reflux by putting pressure on the belly and lower esophagus.
- Lose weight. Whittling the excess pounds can significantly reduce GERD symptoms if you are overweight.
- Stop smoking. Quitting this unhealthy habit is one of the best things you can do to treat symptoms of GERD.
Surgical Treatment
If you require frequent high doses of PPIs to manage your symptoms, experience esophageal damage despite medication, and have a hiatal hernia, you may need to undergo surgery for GERD. However, exploring other treatment options before considering surgery is advisable.
There are various surgical procedures to treat acid reflux. Three common procedures include LINX surgery, transoral incisionless fundoplication (TIF) and fundoplication.
- LINX: LINX surgery involves placing a band of magnetic titanium beads at the junction of the stomach and esophagus. The band of beads allows food to pass through to the stomach, preventing reflux.
- Transoral incisionless fundoplication (TIF): TIF is a less invasive procedure that uses an endoscope (a tiny tube with an attached camera) to wrap the stomach around the lower esophageal sphincter (LES) with plastic fasteners.
- Fundoplication: This surgery involves winding the top of the stomach around the LES to increase pressure in the lower esophagus. This procedure is performed either through laparoscopic surgery (where the surgeon enters the LES area through small holes in the abdomen) or open surgery.
Summary
Heartburn is a common condition that most people experience every once in a while. It is a burning sensation in the chest that usually occurs after eating or at night, and it is caused by stomach acid refluxing into the esophagus. In most cases, heartburn can be managed with lifestyle changes such as avoiding spicy and acidic foods, eating smaller meals, and not lying down immediately after eating.
However, if you’re experiencing heartburn more than twice per week and lifestyle changes are not helping, you may be dealing with Gastroesophageal Reflux Disease (GERD). GERD is a chronic condition in which the stomach acid flows back into the esophagus, causing inflammation and damage to the lining of the esophagus. The symptoms of GERD include heartburn, regurgitation, and difficulty swallowing.
If you have received a diagnosis of GERD, your doctor will help you find a treatment plan that works for you. Treatment options include lifestyle changes, over-the-counter medications, prescription medications, and, in severe cases, surgery.
Don’t let persistent heartburn get in the way of living your life. Talk with a doctor if you believe you may have symptoms of GERD. Remember, early diagnosis and treatment of GERD can prevent complications and improve your quality of life.
Frequently Asked Questions
What is the best treatment for GERD?
If you want to treat GERD symptoms, proton pump inhibitors (PPIs) are a more practical option than H2 blockers. They are also capable of healing the esophageal lining in the majority of GERD patients. You can purchase PPIs without a prescription, or your doctor can prescribe them. Doctors may sometimes recommend long-term use of PPIs to treat GERD.
What is the first line of management for GERD?
For mild symptoms of GERD, lifestyle changes are recommended alongside nonprescription antacids or H2 receptor blockers. Antacids, such as Tums and Rolaids, can neutralize stomach acid and provide short-term relief in relieving heartburn.
Does drinking water help GERD?
Yes. Taking small sips of water throughout the day can help wash away stomach acid in the esophagus and soothe a cough related to GERD.
What foods to avoid if you have GERD?
If you have GERD, it’s best to avoid the following foods and beverages:
- Spicy foods, like chili peppers
- Fatty foods
- Dairy products, like cow’s milk
- Acidic foods and drinks, such as oranges and tomatoes
- Alcohol
- Chocolate
- Coffee
- Carbonated drinks like soda.
What foods neutralize stomach acid immediately?
Non-citrus fruits like bananas can neutralize stomach acid and quickly relieve acid reflux and heartburn due to their natural antacid properties and high pH.
References
1- https://pubmed.ncbi.nlm.nih.gov/23853213/
2- https://www.niddk.nih.gov/health-information/health-statistics/digestive-diseases
3- https://www.who.int/health-topics/obesity#tab=tab_1
4- https://www.asge.org/list-pages/patient-informations/understanding-gastroesophageal-reflux-disease
5- https://pubmed.ncbi.nlm.nih.gov/23305085/
6- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7019431/
7- https://www.ncbi.nlm.nih.gov/books/NBK562200/
8- https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/symptoms-causes
9- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6107529/
10- https://link.springer.com/article/10.1007/s00464-008-9873-4
11- https://pubmed.ncbi.nlm.nih.gov/16646627/
12- https://www.ncbi.nlm.nih.gov/books/NBK525994/
Dr. Matthew Olesiak, MD, is the Chief Medical Director at SANESolution, a renowned wellness technology company dedicated to providing evidence-based solutions for optimal living. Dr. Olesiak earned his medical degree from the prestigious Jagiellonian University Medical College in Kraków, Poland, where he developed a strong foundation in medicine.



