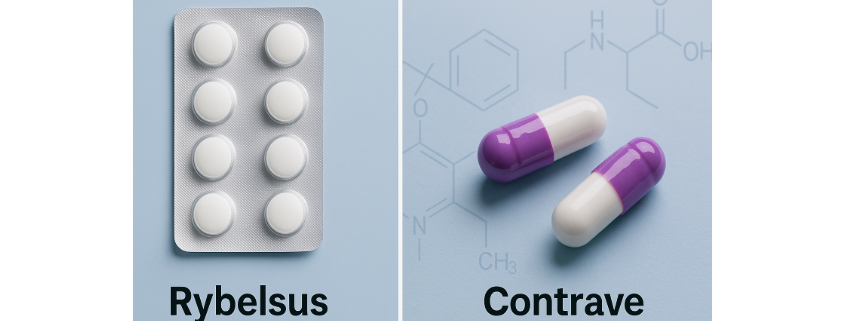
Taking Contrave and Rybelsus Together Drug Interactions

Combining medications for weight loss has become increasingly common, particularly as more people seek medically-supported strategies to manage body weight and improve metabolic health. Two such medications—Contrave and Rybelsus—are gaining attention for their potential effectiveness when taken together. But before combining these weight loss drugs, it’s essential to understand the possible drug interactions, side effects, and risks.
This guide explores what happens when you take Contrave and Rybelsus together, drug interactions, the science behind each medication, their approved uses, potential interactions, and important safety considerations.
Key Takeaways
- Contrave and Rybelsus target weight loss through different mechanisms, but combining them may increase the risk of low blood sugar, nausea, and other side effects.
- The combination may be effective for certain individuals, especially when used with a reduced-calorie diet and lifestyle changes, but only under close medical supervision.
- Your healthcare provider should evaluate your health history, current medications, and risk factors before prescribing both medications together.
Understanding Contrave and Rybelsus
Contrave is a combination medication that includes two active ingredients: naltrexone, which affects the brain’s reward system, and bupropion, which is commonly used to treat depression and aid smoking cessation. Together, they work on appetite and reward centers in the brain to reduce hunger and cravings.
Contrave is available as an extended-release tablet and is FDA approved for chronic weight management in certain adults with a BMI ≥30 or ≥27 and a weight-related condition such as type 2 diabetes or high blood pressure.
Rybelsus, on the other hand, contains the active ingredient semaglutide, a GLP-1 receptor agonist. It mimics a hormone that helps regulate blood sugar and slows gastric emptying, which can promote weight loss and improve blood sugar control.
Rybelsus is also an FDA-approved prescription medication used to manage type 2 diabetes and aid in weight loss in a subset of overweight or obese patients.
Can You Take Contrave and Rybelsus Together?
The combination of Contrave and Rybelsus is not explicitly contraindicated, but it’s not officially approved by the Food and Drug Administration (FDA) for use together, either.
However, doctors may prescribe both under certain conditions based on your health history and risk profile.
“Combining Contrave and Rybelsus may be effective for certain patients struggling with obesity or uncontrolled type 2 diabetes, but it must be approached with caution,” says Dr. Matthew Olesiak, MD, Chief Medical Director at SANE MD. “The potential for drug interactions and overlapping side effects—especially low blood sugar and nausea—requires close monitoring by a healthcare professional.”
This off-label combination targets different mechanisms: Contrave affects neurotransmitters in the brain, while Rybelsus enhances insulin production and slows digestion. For individuals with weight-related conditions, this dual approach may offer added benefit—but only when carefully monitored.
Potential Drug Interactions and Side Effects
Low Blood Sugar (Hypoglycemia)
One of the most notable concerns is the increased risk of low blood sugar, especially in people who take other diabetes medications or insulin. Both Rybelsus and other diabetes medications work to lower blood sugar, which can be compounded when taking additional weight loss medications.
Common symptoms of low blood sugar include dizziness, sweating, confusion, shakiness, and, in severe cases, loss of consciousness. Patients with a personal or family history of diabetes or hypoglycemia may be especially vulnerable.
Gastrointestinal Distress
When taking Contrave and Rybelsus together drug interactions can include nausea, vomiting, constipation, and diarrhea, particularly when first starting. These side effects may be intensified when combining Contrave and Rybelsus.
“Start low and go slow—titration is key when combining multiple weight loss drugs,” says Dr. Olesiak. “Most adverse effects occur early on, and careful adjustment can help patients tolerate the combination better.”
Increased Blood Pressure
Contrave, particularly the bupropion component, can increase blood pressure and heart rate. For individuals with high blood pressure or heart disease, this may raise the risk of serious cardiovascular events.
While some studies have indicated that bupropion may have a neutral or even cardioprotective effect, there is evidence suggesting that bupropion can lead to increases in blood pressure and heart rate, particularly at higher doses.
For instance, a study published in The American Journal of Psychiatry observed that bupropion caused a rise in supine blood pressure among depressed patients with heart disease, although it did not lead to significant conduction complications or exacerbate ventricular arrhythmias. Additionally, the FDA prescribing information for Contrave notes that patients may develop elevated blood pressure or heart rate during treatment, with the risk potentially being greater during the initial three months of therapy.
Therefore, monitoring blood pressure regularly and informing your healthcare provider of any history of heart disease or hypertension is critical.
Suicidal Thoughts and Mental Health
Contrave contains bupropion, which has a boxed warning for suicidal thoughts, especially in younger populations. Patients with a personal or family history of mental illness should proceed with caution and inform their healthcare provider of any mood changes.
Risk Factors to Consider
Before prescribing Contrave and Rybelsus together, a healthcare provider will carefully evaluate a patient’s medical conditions, health history, and current medication regimen. While this combination may be beneficial for certain individuals seeking weight loss, it can also increase the potential for serious adverse effects if not properly monitored.
Several specific factors may make the combination riskier for some people.
1. History of Seizure Disorders
Contrave contains bupropion, a prescription medication known to increase the risk of seizures, particularly in individuals with a personal or family history of seizure disorders. Taking Contrave in combination with other prescription drugs that lower the seizure threshold—such as Suboxone, or in high doses—can be dangerous.
People with conditions like epilepsy, severe head trauma, or those withdrawing from alcohol or sedatives should not take Contrave.
2. Thyroid Tumors or Family History of Medullary Thyroid Carcinoma
Rybelsus (semaglutide) carries a boxed warning for the potential development of thyroid tumors, including medullary thyroid carcinoma, based on findings from animal studies. Individuals with a personal or family history of this rare cancer—or those with multiple endocrine neoplasia syndrome type 2 (MEN 2)—should avoid taking Rybelsus.
Regular monitoring and clear communication about thyroid-related symptoms, such as neck swelling or difficulty swallowing, are essential during treatment.
3. Existing Liver Problems
Both Contrave and Rybelsus are metabolized through the liver. Individuals with moderate to severe liver problems may experience impaired drug clearance, which can lead to accumulation and increased risk of side effects.
Your doctor may adjust dosages or recommend alternative weight loss drugs depending on liver function tests and overall liver health.
4. History of Suicidal Thoughts or Mental Health Disorders
Because Contrave includes bupropion—an antidepressant—there is a most solemn warning regarding the risk of suicidal thoughts and behaviors, especially among young adults and those with mood disorders. Patients with a known personal or family history of depression, anxiety, or past suicide attempts should be closely monitored.
Any emerging mood changes, agitation, or worsening mental health should be reported immediately to a healthcare professional.
5. Current Use of Other Medications
Interactions with other drugs are a key concern when combining Contrave and Rybelsus. In particular, medications that affect dopamine levels (dopaminergic drugs), other diabetes medications, antidepressants, like Paxil, and medications that can increase blood pressure or heart rate, such as Vyvanse, may increase the risk of serious complications.
It’s critical to disclose all prescription medications, over-the-counter drugs, and supplements you’re taking.
6. Use of Other Diabetes Medications or Insulin
Rybelsus is often prescribed for blood sugar control in type 2 diabetes, and combining it with other diabetes medications or insulin can increase the risk of low blood sugar. Symptoms such as shakiness, confusion, dizziness, or fainting should be taken seriously.
A tailored treatment plan that includes close monitoring of blood sugar levels is crucial when using multiple diabetes medications together.
7. Previous Allergic Reactions to Any of the Active Ingredients
Patients who have experienced allergic reactions to semaglutide, bupropion, or naltrexone should not take Rybelsus or Contrave. Reactions can range from mild rash to serious, life-threatening conditions like anaphylaxis.
Symptoms of a severe allergic reaction may include hives, difficulty breathing, chest tightness, or swelling of the face or throat. These signs require immediate emergency medical attention—patients should stop the medication and call 911 or their local emergency services number right away.
Overall, before starting any combination of weight loss drugs, it’s essential to consider your health history, medical conditions, and any other medications you’re using. A shared decision-making process with your healthcare provider ensures your treatment is safe, effective, and aligned with your long-term goals for weight management and health improvement.

Weight Loss Benefits and Effectiveness
Although combining Contrave and Rybelsus is not officially recommended by the Food and Drug Administration, some doctors prescribe both when a single medication doesn’t deliver adequate results. This approach can be especially beneficial for individuals with a high starting body weight, obesity-related medical conditions, or those already using other diabetes medications.
The goal of this combination is to influence both appetite regulation and blood sugar control, leveraging different mechanisms to more effectively promote weight loss.
A 2024 retrospective cohort study published in the International Journal of Obesity found that adding bupropion/naltrexone to GLP-1 analogue therapy led to significantly greater weight loss, even among patients who were initially non-responsive to GLP-1 therapy alone (Naude et al., 2024).
Rybelsus helps regulate insulin secretion, delay gastric emptying, and curb appetite by acting on GLP-1 receptors, which supports both aiding weight loss and controlling blood glucose levels. Contrave, meanwhile, targets the brain’s reward system and hunger cues by combining two active ingredients—bupropion and naltrexone.
When taken together under supervision, they may offer complementary benefits: Rybelsus enhances satiety and blood sugar balance, while Contrave works to reduce cravings and emotional eating triggers.
Both medications have been proven in clinical trials to support significant weight loss, particularly when paired with a reduced-calorie diet, regular physical activity, and consistent lifestyle changes. For some individuals, this combination may result in more weight loss than using either medication alone, especially when previous efforts have failed to produce sustained results.
Clinical Trial Data
- In one pivotal trial published in the New England Journal of Medicine, semaglutide (Rybelsus) led to weight loss of up to 14% of participants’ body weight over a 68-week period. These outcomes were most notable in patients who adhered to treatment guidelines and engaged in lifestyle interventions.
- Contrave’s clinical trials demonstrated an average weight loss of approximately 4–5% over one year, particularly when used alongside structured behavioral support and nutritional counseling, as reported by FDA Access Data.
- For individuals with obesity or overweight with weight-related conditions such as high blood pressure or type 2 diabetes, these medications have also shown improvements in metabolic markers, including blood sugar, triglycerides, and waist circumference, according to the New England Journal of Medicine.
It’s important to note that individual results can vary. Factors like adherence to medication, dietary patterns, physical activity levels, medical conditions, other drugs in use, and starting body weight all influence how much weight loss a person may achieve. Some patients may lose a modest amount, while others could experience more dramatic changes over time.
In summary, although not officially approved to be taken in tandem, Contrave and Rybelsus may offer enhanced benefits for weight management when used cautiously together. However, this should only be considered after consultation with a qualified healthcare provider, and with close monitoring for side effects such as low blood sugar, increased blood pressure, or gastrointestinal discomfort.
When part of a comprehensive treatment plan, this combination may be a useful option for patients struggling with obesity or weight-related conditions who haven’t had success with a single agent alone.
Comparing Contrave vs. Rybelsus
Some patients may wonder about Contrave vs Rybelsus in terms of effectiveness. While both are weight loss drugs, they work differently:
| Medication | Active Ingredient(s) | Primary Action | FDA Approval |
|---|---|---|---|
| Contrave | Naltrexone + Bupropion | Reduces appetite & cravings | Weight management |
| Rybelsus | Semaglutide | Regulates insulin, delays gastric emptying | Type 2 diabetes & off-label weight loss |
When comparing Contrave vs Rybelsus, the decision depends on your medical conditions, goals, and potential risks. Some patients respond better to one medication, while others may need a combination.
Insurance Coverage and Access
Access to these prescription drugs can be limited by insurance coverage. Many insurers require prior authorization or limit how long weight loss medications can be used. Discuss these restrictions with your healthcare provider or pharmacist when starting treatment.
Some telemedicine platforms offer free and confidential support when navigating insurance or finding the right prescription medication. Under the guidance of a provider, you may also consider over-the-counter alternatives or generics.
Monitoring and Ongoing Care
Patients using Contrave and Rybelsus together require regular follow-up to monitor for:
- Changes in blood sugar
- Blood pressure levels
- Emerging side effects or adverse effects
- Signs of liver problems or thyroid tumors
Your healthcare provider may adjust doses, pause treatment, or discontinue one medication if needed. Never stop or change medications without medical supervision.
Doctors typically start with low doses and increase gradually to reduce side effects and avoid interactions with other drugs or similar drugs.
Warnings and Precautions
FDA Boxed Warnings
- Contrave carries a boxed warning for suicidal thoughts and behavior, particularly in younger adults.
- Rybelsus has a boxed warning about the potential risk of thyroid tumors, including medullary thyroid carcinoma, based on animal studies.
These warnings highlight the importance of open communication with your doctor, especially if you have a family history of mental illness or thyroid cancer.
When to Seek Help
If you experience severe side effects, symptoms of low blood sugar, chest pain, mood changes, or allergic reactions, contact your provider immediately. In life-threatening situations, call your local emergency services number.
Those struggling with mood disorders can speak with a volunteer crisis counselor or mental health provider for free and confidential support. Don’t wait to seek support—your safety and well-being come first.
Frequently Asked Questions (FAQ)
Combining medications for weight loss or diabetes management can be effective, but it’s essential to understand potential interactions and risks.
Below are answers to common questions about using semaglutide (Rybelsus) and Contrave, including who may benefit and who should proceed with caution.
1. Can I take semaglutide and Contrave together?
Yes, semaglutide (the active ingredient in Rybelsus) and Contrave can be taken together in some cases, but only under the guidance of a healthcare provider. Both medications are prescription drugs used to promote weight loss through different mechanisms—semaglutide helps with blood sugar control and satiety, while Contrave targets appetite and reward pathways in the brain.
However, combining them may increase the risk of low blood sugar, nausea, and other side effects, particularly in people also taking other diabetes medications. Your provider will consider your health history, medical conditions, and current medications to determine if this combination is safe for you.
2. What medication should not be taken with Rybelsus?
Rybelsus (semaglutide) should not be combined with other GLP-1 receptor agonists or certain other diabetes medications without medical supervision. These combinations can lead to low blood sugar or gastrointestinal side effects. Rybelsus may also interact with prescription medication that affects gastric motility or absorption.
Additionally, patients with a history of medullary thyroid carcinoma, thyroid tumors, or multiple endocrine neoplasia syndrome type 2 should avoid Rybelsus due to its boxed warning. Always review your full medical conditions and medication list with your healthcare provider before starting Rybelsus.
3. What medications should not be taken with Contrave?
Contrave should not be taken with monoamine oxidase inhibitors (MAOIs), certain dopaminergic drugs, or other medications that lower the seizure threshold, due to the increased risk of seizures. Contrave drug interactions may also occur with drugs used to treat depression, other drugs that affect blood pressure or heart rate, and medications that contain bupropion or naltrexone.
Individuals with seizure disorders, eating disorders, or those undergoing abrupt alcohol or sedative withdrawal should not use Contrave. Always discuss your health history, including any other medications, with your healthcare provider.
4. Can diabetics take Contrave?
Yes, some individuals with type 2 diabetes may benefit from taking Contrave, especially if they struggle with weight management. However, caution is required since Contrave can interact with other diabetes medications, potentially leading to low blood sugar or increased blood pressure. Diabetics with seizure disorders, liver problems, or certain mental health conditions may not be ideal candidates.
It’s essential that a healthcare professional evaluates your case and monitors your blood sugar and blood pressure regularly during treatment.
Final Thoughts
Combining Contrave and Rybelsus together for weight loss is a promising but complex approach. It may benefit some individuals struggling with obesity, blood sugar control, or other weight-related conditions—but only when used under the supervision of a knowledgeable healthcare provider.
With potential risks like low blood sugar, increased blood pressure, and drug interactions, a comprehensive health evaluation is critical. By understanding the pros and cons, monitoring your response closely, and maintaining regular medical check-ins, you can make informed decisions about your path to better health.
Sources
The American Journal of Psychiatry
International Journal of Obesity
New England Journal of Medicine
New England Journal of Medicine

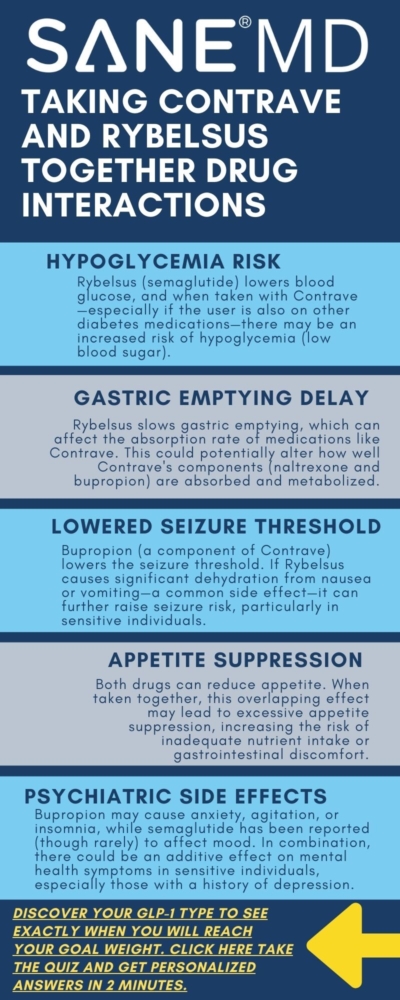
Contrave and Buspar Drug Interactions: Safe to Combine?

Combining medications can sometimes lead to unintended consequences. For individuals using Contrave for weight loss and Buspar (buspirone) for anxiety, it’s important to understand how these two drugs might interact. While both can be helpful in managing separate conditions, certain drug interactions may increase the risk of side effects, reduce effectiveness, or require monitoring by a healthcare provider.
This article takes an objective look at Contrave and Buspar drug interactions, with guidance on how to take both medications safely—if at all. We’ll cover known risks, overlapping side effects, and what to discuss with your health care professional before starting or combining these prescriptions.
Key Takeaways
- Combining Contrave and Buspar may increase the risk of side effects such as dizziness, confusion, and blood pressure changes.
- Patients with a history of seizures, mental health changes, or high blood pressure should consult a healthcare professional before combining these medications.
- Careful monitoring and potential dosage adjustments may be needed when taking Contrave and Buspar together.
What Is Contrave?
Contrave is a prescription medication approved for chronic weight management in certain adults with a BMI over 30—or over 27 with a weight-related health condition such as type 2 diabetes or high blood pressure. It combines two active ingredients: naltrexone hydrochloride and bupropion hydrochloride, each with unique effects on the brain.
- Bupropion is an antidepressant also used to help patients quit smoking and treat depression.
- Naltrexone is traditionally used to treat alcohol and opioid withdrawal.
Together, these compounds target hunger and cravings in the brain. To achieve maximum results, patients taking Contrave are encouraged to follow a reduced-calorie diet and increase physical activity.
What Is Buspar?
Buspar, the brand name for buspirone, is an anti-anxiety medication. Unlike benzodiazepines, Buspar does not cause sedation or dependency. It works by affecting serotonin and dopamine receptors in the brain, and is often used to treat generalized anxiety disorder.
Buspar is typically taken multiple times a day and may take several weeks to become effective. It’s generally well-tolerated but can cause side effects like dizziness, headaches, nausea, and restlessness.
While there’s no official contraindication that forbids taking Contrave and Buspar together, combining these medications may increase the risk of certain side effects or cause overlapping central nervous system (CNS) effects, such as:
- Dizziness
- Drowsiness
- Confusion
- Difficulty concentrating
- Increased blood pressure
Both medications influence brain chemistry. Contrave affects norepinephrine and dopamine, while Buspar acts mainly on serotonin receptors. In rare cases, this could lead to serotonin syndrome, a potentially life-threatening condition. Symptoms of serotonin syndrome include agitation, rapid heartbeat, hallucinations, and trouble breathing.
“There’s no blanket answer for whether it’s safe to take Contrave and Buspar together,” says Dr. Matthew Olesiak, Chief Medical Director at SANE MD. “It depends on the patient’s full medical history, current medications, and health goals. A health care professional must evaluate all risks and benefits before prescribing both drugs at once.”
Risk Factors to Consider
1. Seizure Risk
One of the most serious concerns when taking Contrave is its well-documented risk of seizures. This risk is primarily linked to bupropion hydrochloride, which is known to lower the seizure threshold—especially at higher doses or in individuals with specific medical conditions. People with a history of seizures, head injury, eating disorders (such as anorexia nervosa or bulimia), or those who suddenly stop drinking alcohol are at significantly higher risk. Additionally, concurrent use of over-the-counter drugs or stimulants that impact the nervous system, such as modafinil, or lower the seizure threshold, such as Tramadol and codeine, may exacerbate the issue.
Although Buspar (buspirone) is not typically associated with seizures, it does have effects on the central nervous system and may interact in unpredictable ways when combined with Contrave. The increased risk is particularly concerning in those with a neurological history or other health conditions that influence brain function. This potential interaction qualifies as one of several drug interactions that necessitate caution and close medical supervision.
Before starting Contrave treatment, patients should discuss any past head injury, loss of consciousness, or seizure activity with their health care professional. A detailed health history is critical, especially if you’re also taking other drugs that influence neurological activity. If a seizure occurs, taking Contrave should be discontinued immediately, and medical help should be sought.
2. Mental Health Changes and Suicidal Thoughts
Another major safety concern associated with Contrave is the boxed warning that alerts doctors about the risk of suicidal thoughts and mental health changes. These adverse reactions are especially likely in younger adults and during the first few months of therapy or during dosage adjustment. As bupropion is an antidepressant, it can cause behavioral shifts, particularly in those with pre-existing psychiatric diagnoses.
Buspar is often prescribed to treat depression and generalized anxiety disorder. While it tends to be well-tolerated and non-sedating, it still alters neurotransmitter activity—particularly involving serotonin. When paired with Contrave, the overlapping effects on dopamine, norepinephrine, and serotonin can increase the risk of emotional volatility or destabilize existing mental health conditions. See our guide to learn how Contrave can be used for depression.
This is particularly dangerous in patients with bipolar disorder, where certain medications can trigger manic episodes or deepen depressive ones. Additionally, if you or a family member has a history of mental health disorders, suicidal behavior, or mood swings, this should be discussed before combining these medications.
It’s essential to be aware of early warning signs, such as sudden mood changes, aggression, insomnia, impulsivity, or worsening depression. If you notice these behaviors while taking Contrave or after starting Contrave treatment, consult your healthcare provider immediately. Regular check-ins during the initial months of Contrave treatment can help prevent the escalation of symptoms.
3. Blood Pressure Changes
High blood pressure is a known side effect of Contrave and should not be taken by individuals with uncontrolled hypertension, according to the FDA-approved prescribing information.
Bupropion, by increasing norepinephrine levels, can lead to elevated blood pressure and heart rate, especially during the start of treatment phases or when combined with other drugs affecting cardiovascular function.
Buspar, while generally benign regarding cardiovascular effects, can occasionally cause fluctuations in blood pressure, particularly in those sensitive to changes in stress hormones or CNS stimulants. When used in combination with Contrave, there’s a potential increased risk of cardiovascular side effects, including rapid heartbeat, chest discomfort, and dizziness.
The concern is even greater in patients already dealing with high blood pressure or those using medications to manage it. Buspirone may also interact with certain over-the-counter medications, like decongestants, that can further elevate blood pressure or heart rate. These Contrave interactions are often overlooked but could result in serious injury if not properly managed.
“If you’re taking Contrave and notice symptoms like rapid heartbeat, chest pain, or blurred vision, talk to your doctor immediately,” adds Dr. Olesiak. “These could be signs of high blood pressure or other serious complications that require dosage adjustment or discontinuation.”
Routine monitoring of blood pressure is essential throughout the course of Contrave treatment, especially if you are also using Buspar or any other drugs that impact cardiovascular function. Keep track of symptoms and follow all guidance in the medication guide or patient package insert.
Overlapping Side Effects
Taking Contrave and Buspar at the same time may increase the risk of shared or enhanced side effects. Both medications act on the brain and nervous system, which can lead to cumulative effects in certain individuals.
Common overlapping side effects of Contrave and Buspar include:
- Nausea or vomiting
- Headaches
- Dry mouth
- Dizziness
- Sweating
- Tremors
- Insomnia or restlessness
These symptoms can vary in intensity but may be more disruptive during the early stages of taking Contrave or when initiating a new dose adjustment. For some patients, side effects like tremors, nausea, or dizziness can impair driving or routine activities, increasing the risk of accidents or falls—especially in older adults.
In a smaller subset of patients, more serious complications may develop. These include serious skin reactions, a broad category that encompasses conditions like Stevens-Johnson syndrome or toxic epidermal necrolysis—both of which are life-threatening and require emergency care.
Signs of a serious skin reaction may include:
- Skin rash or blistering
- Peeling skin
- Red or purple lesions
- Fever
- Sore throat
Additionally, signs of an allergic reaction include swelling of the face or throat, trouble breathing, severe itching, or eye pain. These symptoms require immediate cessation of medication and urgent medical care.
If you experience any of these symptoms—particularly swelling, hives, or labored breathing—call your local emergency number right away. These could indicate a medical emergency and should never be ignored. Let your provider know if you’ve ever had an allergic reaction to medications in the past, including weight loss drugs or medications used to treat alcohol or mood disorders.
Because these symptoms may also occur with systemic exposure to other medications or environmental allergens, it’s critical to have a full understanding of your health factors and any behaviors Contrave may amplify. In rare cases, even lab tests may be needed to determine the cause of your reaction or confirm drug safety.

Who Should Avoid Combining These Drugs?
The combination of Contrave and Buspar should be avoided or used with caution in people with:
- History of seizures or head injury
- Diagnosed bipolar disorder
- Uncontrolled high blood pressure
- History of eating disorders
- Recent use of monoamine oxidase inhibitors
- Current use of opioids (due to naltrexone and bupropion effects)
Additionally, people who suddenly stop drinking alcohol or who are undergoing opioid withdrawal face an increased risk of adverse reactions when taking Contrave, according to the FDA-approved prescribing information.
This risk may be compounded if Buspar is also involved.
Considerations When Taking Contrave
Contrave is provided in extended-release tablets, which should not be crushed, chewed, or split. Doing so may alter the absorption rate, leading to an increased risk of side effects. It is also important to avoid high-fat meals when taking Contrave, as they may increase the risk of seizure by raising drug levels in the blood.
Contrave is not recommended for use with certain other drugs—including over-the-counter stimulants, psychiatric medications, and weight loss supplements. Make sure your health care professional knows about all medications and supplements you take, including vitamin interactions or over-the-counter drugs.
You’ll also want to keep track of:
- Missed dose instructions (do not double up)
- Patient package insert and medication guide updates
- Changes to mental health, mood, or energy
- Whether you are pregnant or breastfeeding (breast milk transfer risk)
Blood Sugar and Caffeine Considerations
For individuals with diabetes or metabolic conditions, Contrave treatment may lower blood sugar levels. This could pose a danger if you’re also taking Buspar, which can sometimes cause dizziness or lightheadedness.
Hypoglycemia (low blood sugar) can mimic side effects of both medications, making it harder to determine the cause. Regular blood sugar monitoring and adjustment to any insulin or diabetes medications are advised.
Contrave has been shown to reduce hemoglobin A1c and fasting glucose levels in people with type 2 diabetes, according to FDA-approved clinical data, which may result in low blood sugar for some individuals.
Patients should also avoid excessive caffeine intake. Both drugs can cause insomnia, jitteriness, or restlessness—effects that may be amplified with high doses of caffeine.
How to Safely Start Treatment
Starting Contrave treatment—especially when combining it with Buspar—requires thoughtful planning and clear communication with your health care professional. Because both medications affect the central nervous system and can influence mood, blood pressure, and energy levels, it’s important to take a proactive, informed approach from the very beginning.
Before starting Contrave and Buspar together:
- Review your health history and health conditions with your provider. This includes any past or current issues such as high blood pressure, bipolar disorder, mental health diagnoses, seizures, or eating disorders. Full disclosure of your medical conditions helps your doctor determine whether it’s safe to combine these drugs or if alternative treatments are a better fit.
- Ask about potential Contrave interactions with other drugs, supplements, or foods. Both prescription and over-the-counter medications—including vitamins, herbal products, and cold medicines—may interact with naltrexone and bupropion, leading to adverse reactions or reduced effectiveness. Your provider can help identify certain drug interactions and review the medication guide or patient package insert for up-to-date safety guidance.
- Be honest about your use of alcoholic beverages and whether you plan to quit smoking. People who suddenly stop drinking alcohol or are actively detoxing from opioid withdrawal may face an increased risk of seizures or mood instability while on Contrave. Additionally, bupropion hydrochloride is sometimes used to help quit smoking, so the dosage must be carefully tailored to avoid overlapping effects or accidental duplication.
- If needed, request a dosage adjustment or consider staggering medication start times. Your doctor may recommend slowly introducing Contrave while maintaining a stable Buspar regimen, especially if you’ve recently made changes to your mental health medications. This approach allows your body to adjust gradually and reduces the likelihood of serious side effects, such as the risk of seizures, high blood pressure, or worsening mental health symptoms.
Your doctor will evaluate whether to prescribe Contrave based on a combination of factors, including your health conditions, current treatments, lifestyle, and long-term goals for chronic weight management. They may also monitor for warning signs like skin rash, low blood sugar, or trouble breathing, and recommend regular check-ins during the early phases of taking Contrave.
If you’re already on Buspar, your provider might choose to introduce Contrave using a step-up approach—starting with the lowest dose of extended-release tablets and gradually increasing it over several weeks. This titration helps limit side effects and allows your provider to intervene early if contrave-interaction symptoms appear.
In all cases, clear and ongoing communication with your healthcare provider is key. Report any new symptoms, emotional changes, or difficulties tolerating the medication. Whether your goal is to lose weight, reduce anxiety, or improve your quality of life, a safe and strategic start sets the foundation for long-term success.
Frequently Asked Questions (FAQ)
Combining medications can be confusing, especially when managing multiple health conditions like anxiety, depression, or obesity.
Below are answers to common questions related to Contrave, Buspar (buspirone), and their possible interactions. Always consult your health care professional before starting, stopping, or combining any medications.
1. What medications should not be taken with Contrave?
Contrave should not be taken with monoamine oxidase inhibitors (MAOIs), as this combination can cause dangerous spikes in blood pressure or other severe reactions. Contrave drug interactions can also occur if used with other forms of bupropion, including those used to quit smoking (like Zyban), because doing so may increase the risk of seizures. Contrave should not be taken with benzodiazepines like Xanax without medical supervision, as the combination may lead to dangerous interactions.
Additionally, opioid medications must be stopped at least 7–10 days before starting Contrave due to the naltrexone component, which can cause opioid withdrawal. Use caution with over-the-counter drugs, stimulant-containing products, and medications that may raise blood pressure or impact seizure threshold.
2. Can you take bupropion and BuSpar together?
In some cases, bupropion and Buspar may be taken together under medical supervision, but this combination requires caution. Both drugs affect brain chemistry and may increase the risk of side effects such as dizziness, confusion, anxiety, or even serotonin-related complications. People with a history of mental health conditions, seizures, or high blood pressure should be closely monitored.
Your provider may recommend dosage adjustment or staggered administration to minimize overlapping side effects.
3. What medications cannot be taken with BuSpar?
Buspar should not be combined with MAO inhibitors, as this may lead to dangerously high blood pressure. It also interacts with serotonergic drugs, increasing the risk of serotonin syndrome—a rare but serious condition. Use caution with antidepressants, antipsychotics, certain antibiotics (like linezolid), and even herbal products like St. John’s Wort.
Always disclose your full medication list, including over-the-counter and vitamin interactions, to your healthcare provider before starting treatment with Buspar.
4. Can I take Contrave if I take bupropion?
Contrave already contains bupropion hydrochloride, one of its two active ingredients. If you’re already taking bupropion for treating depression, smoking cessation, or another reason, taking Contrave at the same time could cause dangerously high bupropion levels and significantly increase the risk of seizures. Your doctor may recommend switching to Contrave or adjusting your dose, but you should never take both at the same time without professional guidance.
Be especially cautious if you have a history of head injury, eating disorders, or use alcoholic beverages regularly.
The Bottom Line
Combining Contrave and Buspar can be safe for some patients, but it carries real risks—especially if you have medical conditions like high blood pressure, a history of seizures, or current mental health challenges.
Speak with a trusted healthcare provider about the safest path forward. Do not attempt to mix or adjust medications without professional input. If you suspect an adverse reaction, reach out to your doctor or call your local emergency number immediately.
When taken carefully and with oversight, both medications can play a role in achieving better health—whether that means managing anxiety, supporting chronic weight management, or helping you lose weight safely.
SOURCES

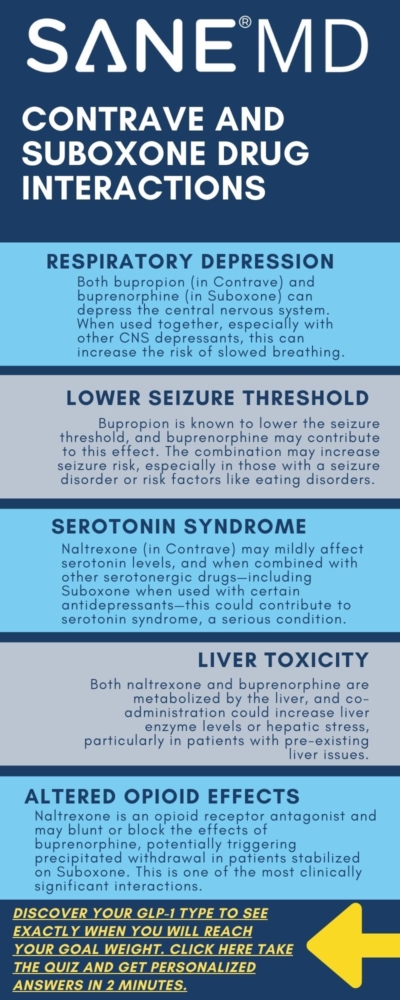
Contrave and Suboxone Drug Interactions: Dangerous Combo?

Combining medications always requires caution, especially when the drugs affect the brain’s reward system, metabolism, and pain pathways. Contrave and Suboxone are both powerful prescription treatments used for different health conditions—weight loss and opioid dependence, respectively—but their effects can overlap in ways that may not be safe.
This article explores the potential Contrave and Suboxone drug interactions, breaking down what you need to know about risks, symptoms, and how to talk to your doctor if you’re currently prescribed or considering treatment with either of these drugs.
Key Takeaways
- Combining Contrave and Suboxone may increase the risk of central nervous system depression, seizures, withdrawal symptoms, and liver stress.
- These two medicines should not be used together without close monitoring by a healthcare provider familiar with both.
- People with mental health conditions, eating disorders, or a seizure disorder face a higher risk when using either medication, especially in combination.
Understanding Contrave and Suboxone
Contrave is an FDA-approved combination of bupropion (also known by the brand Wellbutrin SR) and naltrexone, used to support weight loss in certain adults with obesity or weight-related health conditions. It works by acting on areas of the brain involved in hunger and cravings.
Suboxone, on the other hand, is a combination of buprenorphine, a partial opioid agonist, and naloxone, an opioid antagonist. It’s prescribed to treat opioid dependence and manage opioid withdrawal.
Both drugs act on the brain’s chemical systems, and both involve extended release tablets in some formulations, which can complicate timing and dosing when used together.
Why This Combo May Be Risky
Combining Contrave and Suboxone may result in complex and potentially harmful drug interactions due to the way each medication affects the brain, liver, and central nervous system. Both drugs are prescribed for serious health conditions—weight loss and opioid dependence, respectively—but when taken together, they can produce unpredictable side effects. The interaction can alter blood pressure, increase the chance of liver problems, heighten the risk of seizures, and trigger dangerous withdrawal symptoms or mental health conditions.
Below are the most concerning risks associated with taking these two medicines at the same time.
1. Central Nervous System Depression
While bupropion, one of Contrave’s main ingredients, is typically a mild stimulant used to treat depression, Suboxone contains buprenorphine, which has sedative properties that can suppress the central nervous system. When used together, the push-pull effect on brain activity can cause a rollercoaster of symptoms—some individuals may feel overly stimulated, while others experience profound drowsiness, confusion, or even episodes of dissociation. It’s important to note that taking opioids like morphine or codeine with Contrave can have the same effect on the central nervous system.
In rare cases, this combination may lead to impaired motor control or slowed breathing, especially if other medications or alcohol are also in the system.
“Mixing medications that target the brain’s dopamine and opioid receptors increases the complexity and risk. It’s not something patients should attempt without close supervision,” says Dr. Matthew Olesiak, MD, Chief Medical Director at SANE MD.
These neurological effects may be magnified in older adults or anyone with mental health conditions, a history of depression, or sensitivity to psychiatric medications. Always consult your doctor before combining Contrave with any other drugs affecting the nervous system.
2. Seizure Risk
Contrave may increase the risk of seizures, particularly in individuals with a seizure disorder, eating disorders, or those who drink alcohol regularly. Bupropion alone has a known dose-dependent seizure risk, which is why it’s often contraindicated in individuals with predisposing factors. Meanwhile, Suboxone can occasionally lower the seizure threshold, although this is a rare side effect.
When combined, these effects may increase the risk of neurological instability, especially during treatment initiation or dosage changes.
Many studies, including one published by the Canadian Medical Association Journal (CMAJ), found strong evidence that bupropion can lower the seizure threshold, making a seizure more likely.
This concern is heightened during opioid withdrawal, when the brain is already under stress from chemical fluctuations. Symptoms such as muscle twitching, disorientation, or unusual tiredness should be reported to your healthcare provider immediately.
Patients who are also on other medications that affect the brain may face a higher risk of complications.
3. Liver Strain
Both Contrave and Suboxone are metabolized through the liver, and prolonged or combined use can increase the workload on this vital organ. Contrave may increase the risk of liver damage, especially when used in patients who drink alcohol or are taking other medications processed by hepatic enzymes. Suboxone has also been linked to elevated liver enzymes, indicating potential stress or damage.
Taking the two together may compound the toxic burden, resulting in serious complications over time.
Symptoms of liver problems include:
- Dark urine
- Pale stools
- Unusual tiredness
- Skin rash
- Pain in the upper right abdomen
Indeed, a study published in the Annals of Pharmacotherapy demonstrated that Suboxone can elevate liver enzymes, especially when taken intravenously, potentially causing liver damage.
Individuals with pre-existing medical conditions like hepatitis, fatty liver disease, or those who take over-the-counter pain relievers frequently are especially vulnerable.
If you develop any of these symptoms, you should seek medical attention without delay.
4. Risk of Precipitated Withdrawal
One of the most serious dangers of combining Contrave and Suboxone is the possibility of precipitated withdrawal—a sudden onset of severe opioid withdrawal symptoms triggered by naltrexone, which blocks opioid receptors.
If a patient is still physically dependent on opioids or currently taking Suboxone, the presence of naltrexone can override the stabilizing effects of buprenorphine, resulting in immediate and intense withdrawal symptoms.
These symptoms may include:
- Muscle aches
- Chills and sweating
- Vomiting or diarrhea
- Mood swings or irritability
- Anxiety or suicidal thoughts
This effect not only causes immense discomfort but may also lead to relapse in individuals trying to overcome opioid dependence. That’s why most healthcare providers require a full detox period before starting Contrave in any patient with a history of opioid use. Skipping this step can increase the risk of a life-threatening situation, particularly in unsupervised settings.
5. Overlapping Side Effects and Mental Health Impact
Each medication carries its own risk profile for psychiatric symptoms, but the risks may multiply when they’re taken together. Both drugs can affect mood and cognition—Contrave may contribute to anxiety, irritability, or suicidal thoughts, while Suboxone has been associated with emotional blunting and, in some cases, false beliefs or paranoia. It’s important to note that taking Contrave with Buspar can also trigger anxiety and other side effects.
For patients with a history of depression, bipolar disorder, or other mental health conditions, the combination may destabilize mood regulation and cloud judgment.
Additional overlapping side effects include:
- Low blood sugar, especially in patients with diabetes
- Unusual tiredness or lethargy
- Nausea and gastrointestinal discomfort
- Persistent skin rash
- Confusion or hallucinations
These effects can be exacerbated by high-fat meals, polypharmacy (use of multiple other medications), or underlying medical conditions like liver damage or seizure disorders. Monitoring these signs closely during the first few weeks of treatment is crucial, especially for older adults or any vulnerable age group.
Important Considerations Before Taking Contrave with Suboxone
Before starting any new treatment, especially involving prescribed medications like Contrave and Suboxone, it’s essential to understand how the combination may affect your body. Both drugs are powerful and act on different systems, but when used together without proper oversight, the risk of complications increases substantially.
Below are the critical steps you should take to stay safe and avoid potentially serious health issues.
Talk to Your Doctor First
Never combine Contrave with Suboxone—or any other medications—without first discussing it thoroughly with your doctor or healthcare provider. This step is vital because your provider will evaluate the full picture of your medical conditions, lifestyle, and past medication use to identify potential drug interactions or health risks.
Some of the factors your provider will review include:
- Your history of seizures or seizure disorder
- Whether you drink alcohol regularly
- Any mental health conditions, such as bipolar disorder or depression
- Use of over-the-counter supplements, herbs, or other drugs
- Past experience with opioid withdrawal or opioid dependence
- Current or recent use of CNS-active agents such as sedatives, stimulants, or other antidepressants
“The risk isn’t just theoretical—it’s well documented. When prescribing Contrave, I ask about current or past use of opioid antagonists, mood stabilizers, and any other CNS-active drugs,” says Dr. Olesiak.
This conversation is especially important if you’re considering starting Contrave while still on Suboxone or recovering from opioid use. You may need to taper off Suboxone completely before it’s safe to begin a reduced-calorie diet supported by Contrave.
Read the Medication Guide Thoroughly
Every patient should carefully read the medication guide included with both Contrave and Suboxone. These documents outline crucial safety warnings, side effects, dosing schedules, and specific health conditions that may increase the risk of complications. For example, high-fat meals can alter how extended-release Contrave tablets are absorbed, potentially leading to adverse reactions. Similarly, starting Contrave without understanding the presence of naltrexone—a potent opioid antagonist—can result in life-threatening withdrawal symptoms if you’re still dependent on opioids.
Don’t rely solely on internet forums or anecdotal advice. Follow the prescribing information, ask your doctor questions, and make sure you fully understand both medications before combining them.
Watch for These Symptoms
Once you begin taking either medication—or both under medical guidance—you should monitor your body closely for warning signs.
The following symptoms may signal a serious allergic reaction, liver problems, or central nervous system issues, and could indicate that your body is not tolerating the drug interactions well:
- Dark urine or pale stools (potential signs of liver damage)
- A persistent or spreading skin rash
- Sudden onset of withdrawal symptoms, such as shaking, sweating, or intense cravings
- Shortness of breath or difficulty breathing (may signal a serious allergic reaction)
- Chest tightness or pain (could point to a rare but possible heart attack)
- Severe mood changes, aggressive or unusual behavior
- Confusion, hallucinations, or false beliefs
These symptoms should never be ignored. If you experience one or more, especially in the early stages of treatment, seek emergency help or contact your healthcare provider immediately. Delayed action could result in worsening of the condition or long-term harm.

Common Conditions That May Increase the Risk
You may face an increased risk of complications if you:
- Have a seizure disorder
- Are currently detoxing from opioids
- Are trying to quit smoking
- Take other antidepressants
- Have diabetes and are managing low blood sugar
- Follow a reduced calorie diet with high fat meals
- Are dealing with bipolar disorder
- Use over the counter pain relievers or other medications
What to Tell Your Healthcare Provider
Be transparent about:
- All medications (including other drugs and supplements)
- Whether you plan to stop taking Contrave
- If you have a history of mental health conditions
- Any signs of liver problems, such as dark urine or pale stools
- If you are pregnant or breastfeeding (some components pass into breast milk)
This is especially vital before you start treatment with one tablet, then increase to two tablets daily as part of extended release dosing.
When It’s Not Safe to Combine
You should avoid combining Contrave and Suboxone if:
- You are on a monoamine oxidase inhibitor
- You’re in active opioid withdrawal
- You’ve experienced a serious allergic reaction to either drug
- You’ve had liver damage from other medications
- You have uncontrolled high blood pressure
Tips for Safe Use
If your healthcare provider determines that using Contrave and Suboxone together is appropriate for your situation, you should take several critical precautions to minimize risk and ensure safer treatment.
These tips are designed to help you avoid harmful drug interactions, manage side effects, and recognize early warning signs of trouble.
Follow Your Doctor’s Instructions for Dosing
Always take each medication exactly as prescribed. This includes sticking to the dosing schedule, not adjusting the number of one tablet or two tablets taken per day without approval, and following titration instructions when starting Contrave. These medications may come in extended-release tablets, which are meant to be swallowed whole—do not crush or split them.
Improper dosing can increase the risk of side effects, reduce effectiveness, or trigger dangerous events like seizures or withdrawal symptoms.
Avoid High-Fat Meals While Taking Contrave
While on Contrave, it’s important to avoid high-fat meals, as these can increase the medication’s absorption rate and lead to more intense side effects. A spike in bupropion levels could contribute to high blood pressure, dizziness, or a serious allergic reaction.
Stick to a reduced-calorie diet with balanced macronutrients, as recommended by your healthcare provider, to promote weight loss while reducing the chance of complications.
Do Not Suddenly Stop Taking Contrave or Suboxone
Abruptly discontinuing either medication may lead to withdrawal symptoms, worsened mental health conditions, or relapse. Stop taking Contrave or Suboxone only under medical supervision, as your doctor may need to taper your dose gradually to reduce the chance of seizures, mood instability, or other health conditions flaring up.
This is especially important if you’re also on other medications that influence brain chemistry, such as other antidepressants or mood stabilizers.
Report Symptoms Like Unusual Tiredness or Mental Fog
Notify your healthcare provider if you notice unusual tiredness, trouble concentrating, or other new or worsening symptoms. These may indicate problems such as low blood sugar, early signs of liver damage, or a developing allergic reaction.
Catching these effects early can help your doctor make necessary adjustments before serious harm occurs.
Do Not Drink Alcohol While on Either Medication
Both Contrave and Suboxone interact poorly with alcohol. Drinking while on either drug can significantly increase the risk of seizures, sedation, or liver problems such as dark urine, pale stools, and upper abdominal pain.
Additionally, alcohol may worsen mental health side effects such as depression, anxiety, and suicidal thoughts. If you currently drink alcohol, talk to your healthcare provider about safe limits—or whether it’s best to abstain entirely during treatment.
Frequently Asked Questions (FAQ)
Before starting or combining any medications, it’s essential to understand potential risks and interactions. Contrave and Suboxone affect brain chemistry in powerful ways and should not be taken together without explicit approval and oversight from your healthcare provider.
Below are answers to some of the most common questions people have about these medications and their possible interactions.
1. Can you take Contrave and Suboxone?
Taking Contrave and Suboxone together is not recommended without close medical supervision. Contrave contains naltrexone, an opioid antagonist, which can interfere with buprenorphine in Suboxone, potentially triggering severe opioid withdrawal. The combination may also increase the risk of liver stress, seizures, or mental health side effects.
Always talk to your healthcare provider before combining these medications to avoid dangerous outcomes.
2. Can you take Suboxone and bupropion together?
Suboxone and bupropion can be taken together in certain cases, but doing so carries a higher risk of seizures, especially in people with a history of seizure disorders or other medical conditions. Bupropion is a stimulant-like antidepressant that lowers the seizure threshold, and Suboxone may further increase this risk when combined.
Your doctor will weigh the benefits against the risks and monitor for symptoms like unusual tiredness, confusion, or agitation. Do not combine these medications without medical guidance.
3. What medications should not be taken with Contrave?
There are many Contrave drug interactions to be aware of. Here are just a few of them: Contrave should not be taken with opioids, opioid-containing medications, or any drugs that lower the seizure threshold, such as other antidepressants, antipsychotics, or corticosteroids. Avoid using it with monoamine oxidase inhibitors (MAOIs), NSAIDs, certain diabetes medications that increase the risk of low blood sugar, and alcohol. High-fat meals should also be avoided during dosing, as they may increase drug absorption and side effects.
Always provide your doctor with a complete list of prescription, over-the-counter, and herbal medications before starting Contrave.
4. What should you not mix with Suboxone?
Suboxone should not be mixed with alcohol, sedatives, benzodiazepines, or other central nervous system depressants, as the combination may lead to life-threatening respiratory depression. It also interacts with certain antifungal drugs, antibiotics, and antiviral medications that affect liver enzymes. Opioid antagonists like naltrexone can block the effects of Suboxone and may precipitate withdrawal.
Check with your healthcare provider before combining Suboxone with any other medications.
5. What happens if you take naltrexone while on Suboxone?
Taking naltrexone while on Suboxone can cause immediate and intense opioid withdrawal symptoms. Naltrexone is a full opioid antagonist and blocks opioid receptors, effectively reversing the effects of buprenorphine in Suboxone. This can result in nausea, vomiting, muscle cramps, sweating, anxiety, and other uncomfortable or dangerous withdrawal symptoms.
If you are on Suboxone, you should not start naltrexone (or Contrave) until you’ve been fully detoxed under medical supervision.
Final Thoughts
While both Contrave and Suboxone can be effective when used alone under the guidance of a healthcare provider, their combination presents significant safety concerns. Patients with mental health conditions, a seizure disorder, or a history of opioid dependence should exercise extreme caution.
Contrave may be right for some people trying to lose weight as part of a reduced-calorie diet, but not if they’re currently on opioid therapy. The drug interactions are serious enough to require individualized assessment before proceeding.
Always review the prescribing information, read the medication guide, and talk openly with your doctor about your full medical history and goals for treatment.
Sources