Contrave and Methadone Drug Interactions: A Risky Combo?
Dr. Matthew Olesiak, MD, is the Chief Medical Director at SANESolution, a renowned wellness technology company dedicated to providing evidence-based solutions for optimal living. Dr. Olesiak earned his medical degree from the prestigious Jagiellonian University Medical College in Kraków, Poland, where he developed a strong foundation in medicine.

Combining medications can sometimes provide powerful therapeutic benefits. Other times, it can pose serious risks. For individuals prescribed both Contrave and methadone, understanding the potential for interaction is not just helpful—it’s essential.
Both drugs serve important roles in treating specific conditions: Contrave is commonly prescribed for weight loss, while methadone is widely used in treating opioid addiction and managing chronic pain. But using them together can carry important safety concerns.
This article provides a medically accurate, clear-eyed look at Contrave and methadone drug interactions, highlighting when the combination might be helpful, when it might be harmful, and what to discuss with your healthcare provider.
Key Takeaways
- Contrave and methadone can affect each other’s impact on the brain and body, increasing the risk of side effects such as seizures, blood pressure spikes, and respiratory depression.
- Patients with a history of drug addiction, bipolar disorder, or uncontrolled high blood pressure may be at especially high risk when combining these medications.
- Always talk with your doctor or healthcare provider before combining any medication, especially those that affect the central nervous system.
Understanding Contrave and Methadone
What is Contrave?
Contrave is a prescription medication approved for weight loss in certain adults who are at risk of a weight-related medical condition, such as type 2 diabetes or high blood pressure. It’s a drug combination made up of bupropion and naltrexone. Bupropion is also used to treat depression, quit smoking, and reduce cravings. Naltrexone is typically used to treat opioid addiction and alcohol use disorder.
Together, these components help decrease appetite and reduce food cravings, especially when combined with a reduced-calorie diet and increased physical activity to help compatible patients lose weight and manage weight long-term.
What is Methadone?
Methadone is a narcotic medicine used primarily in the treatment of opioid addiction and chronic pain. It works by altering how the brain and nervous system respond to pain.
Methadone is also used to prevent withdrawal symptoms in people who have become dependent on other street drugs, such as heroin.
How Contrave and Methadone May Interact
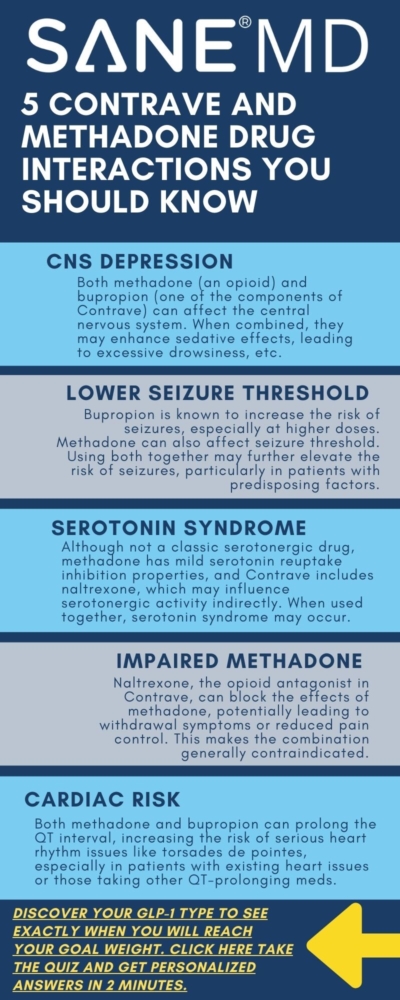
When taken together, Contrave and methadone can result in complex and sometimes dangerous drug interactions, primarily due to the way both affect the brain and central nervous system. Contrave contains bupropion, an atypical antidepressant that also helps certain patients lose weight by suppressing appetite and cravings. Methadone, on the other hand, is a long-acting narcotic medicine that binds to opioid receptors to manage pain or treat opioid addiction.
Bupropion has a well-documented association with increased risk of seizures, particularly at higher doses or in patients with predisposing factors such as eating disorders, head injury, or use of other drugs that lower the seizure threshold, such as alcohol and caffeine. Methadone itself, while not commonly linked to seizures, can cause respiratory depression, sedation, and changes in brain chemistry that may further increase the risk when used in combination.
In addition to the seizure risk, Contrave’s naltrexone component can block opioid receptors. This means that it can reduce or completely negate the effectiveness of methadone, especially in people using methadone for opioid withdrawal or maintenance therapy.
This antagonistic effect can lead to sudden withdrawal symptoms, some of which may require emergency medical attention.
“One of the most concerning risks when combining bupropion and methadone is seizure susceptibility,” explains Dr. Matthew Olesiak, MD, Chief Medical Director at SANE MD. “Methadone alters neurotransmitter levels in the brain, and bupropion may further increase the risk of seizures, especially in individuals with other predisposing factors.”
The interaction becomes even more unpredictable when factoring in other medications a patient might be taking, such as seizure medication, over-the-counter drugs, or antidepressant medicine.
The combined CNS (central nervous system) effects can result in heightened sedation, increased risk of confusion, or erratic mood swings.
Possible Side Effects and Risks
The combination of Contrave and methadone can affect multiple systems in the body, particularly the neurological, cardiovascular, and gastrointestinal systems.
Side effects may be mild in some individuals, but they can also escalate quickly without warning.
Seizures
This is one of the most dangerous risks associated with this drug combination. Bupropion may increase the risk of seizures, especially in patients with a history of head injury, eating disorder, or those taking other medicines that interact with the brain.
Methadone could intensify these effects by disrupting normal brain activity and causing fluctuations in neurotransmitter levels.
Increased blood pressure or uncontrolled high blood pressure
Both medications can raise blood pressure, especially bupropion.
When combined, the risk of developing uncontrolled high blood pressure grows significantly, particularly if patients are also consuming high-fat meals, drinking alcohol, or have a history of hypertension. Our comprehensive guide details how Contrave can increase blood pressure.
Respiratory depression
Methadone is a powerful narcotic medicine that can slow breathing.
If taken in conjunction with other CNS depressants or medications like bupropion, which have stimulating effects, the interaction can be unpredictable—resulting in dangerously slow breathing or sudden apnea in high-risk individuals.
Blurred vision
Changes in vision, such as blurred vision or even eye pain, have been reported in some users of both drugs.
This may be a sign of increased intracranial pressure or other neurological effects and should be addressed promptly.
Dry mouth, stomach pain, or joint pain
These symptoms, while more common and typically less dangerous, may still signal that the body is struggling to metabolize the drug combination effectively.
Persistent stomach pain or joint pain should prompt a consultation with a healthcare provider.
Suicidal thoughts or panic attacks
Patients with underlying mood disorders or taking these drugs to treat depression may experience worsening symptoms.
The risk of suicidal thoughts, panic attacks, and emotional volatility may be increased when Contrave and methadone are used together, especially without careful psychiatric monitoring.
Opioid withdrawal symptoms
Since Contrave includes naltrexone, it can block the effects of methadone.
This blocking can trigger acute opioid withdrawal, with symptoms ranging from agitation and nausea to chest pain, trouble sleeping, and even seizures.
Skin rash, serious skin reactions, or severe skin reaction
Rare, but serious, skin reactions have been linked to both medications.
If a skin rash develops—especially when accompanied by fever, dark urine, or mucosal swelling—it may be a sign of a severe skin reaction requiring immediate medical attention.
Dark urine or eye pain
These may indicate liver strain or neurological side effects and should be reported to your healthcare provider right away.
In rare cases, this combination could lead to a dangerous drug interaction. Since methadone is a full opioid agonist and naltrexone is an opioid antagonist, their effects can directly oppose each other.
This may trigger opioid withdrawal symptoms, especially in patients who are actively dependent on methadone for addiction therapy.
“Naltrexone can block the effects of opioids,” Dr. Olesiak notes. “If someone is taking methadone and starts Contrave without medical guidance, they may experience opioid withdrawal that can be intense and even dangerous. Always talk with your doctor before starting or stopping any medication.”
Who Is at Higher Risk?
1. Individuals with Pre-existing Conditions
People with kidney disease, bipolar disorder, head injury, or an eating disorder may be at greater risk for adverse effects.
For example:
- A person with kidney disease may have trouble clearing the drugs from their body, raising the risk of toxicity.
- Those with bipolar disorder may experience manic episodes triggered by bupropion’s stimulant-like properties.
- Individuals with an eating disorder or history of drug addiction already face a higher risk of seizures, especially when combining CNS-active drugs like Contrave and methadone.
2. People with Mental Health Conditions
Mental health conditions like depression, anxiety, or past trauma can worsen when taking medications that alter mood and brain chemistry. Contrave has been associated with suicidal thoughts, especially in people taking it to treat depression.
Combining it with methadone, especially in those also using antidepressant medicine or seizure medication, may lead to unpredictable mood swings, new or worsening symptoms, and unusual risk-taking behavior.
Even patients in recovery from addiction may relapse or feel destabilized due to the contrasting effects of methadone (which reduces cravings) and naltrexone (which blocks opioids entirely).
3. Patients Taking Other Medications
If you are taking other medicines—especially over-the-counter drugs, weight loss products, or prescription diet pills—you should be extremely cautious. Many over-the-counter medicines for cold symptoms, sleep aids, or pain relief may interact with the central nervous system, amplifying side effects or interfering with drug metabolism.
In addition, patients who drink alcohol regularly may further increase their risk of liver strain, chest pain, serious allergic reactions, or trouble sleeping. Alcohol, methadone, and bupropion all affect brain activity, and combining them could be dangerous.
According to the FDA, combining methadone with CNS depressants—including alcohol and certain medications—can increase the risk of slowed breathing, overdose, and death, and should be managed with extreme caution by healthcare providers. [FDA Drug Safety Communication, 2017]

Warning Signs to Watch For
If you’re taking both medications, it’s essential to monitor for warning signs that may indicate a serious reaction.
Seek emergency medical attention or immediate medical attention if you experience:
- Sudden chest pain
- Severe stomach pain or eye pain
- Signs of a serious allergic reaction (such as swelling of the face, tongue, or throat)
- A severe skin rash or serious skin reaction
- Dark urine, yellowing of the eyes or skin
- Increased blood pressure or symptoms of high blood pressure (like pounding headaches or dizziness)
- Confusion, hallucinations, or panic attacks
Safety Measures and Alternatives
When considering any combination therapy—especially involving medications like Contrave and methadone—it’s essential to take proactive safety steps.
Not everyone will experience side effects, but for those at risk, having safeguards in place can prevent serious complications.
The goal is not just to lose weight or manage pain but to do so safely under the supervision of a trusted healthcare provider.
Talk With Your Doctor
Before starting, stopping, or combining medications, talk with your doctor.
Both Contrave and methadone come with complex pharmacological profiles, and their interaction can result in anything from mild side effects to a dangerous drug interaction.
You should tell your doctor if you:
- Have a personal or family history of seizures, epilepsy, or other neurological disorders. Bupropion, a component of Contrave, is known to increase the risk of seizures, and that risk may be amplified if methadone is added to the mix.
- Are being treated for or have a history of mental illness, including bipolar disorder, panic attacks, or suicidal thoughts. Your provider may need to adjust your treatment plan or monitor you more closely.
- Are pregnant, trying to conceive, or breastfeeding. Both medications have potential implications for your unborn baby, including withdrawal symptoms and developmental risks. Discuss potential alternatives or timing strategies with your healthcare provider.
- Drink alcohol regularly or use street drugs or other street drugs. Alcohol and illicit substances can dramatically increase the risk of side effects like chest pain, confusion, or serious allergic reactions, and interfere with both methadone and Contrave.
- Are using diet pills, supplements, or over-the-counter products. Many of these contain stimulants, depressants, or other compounds that may worsen drug interactions.
- Have weight-related medical problems such as high blood pressure, low blood sugar, or blood sugar instability. These may be affected by changes in appetite, metabolism, or mood caused by either medication.
It’s critical to also disclose whether you are using medications for other conditions—especially seizure medications, heart medications, antidepressant medicines, or any over-the-counter medicines for sleep, pain, or allergies. Certain medicines can increase sedation, spike blood pressure, or alter how your liver processes Contrave or methadone.
When in doubt, bring your prescription label, supplement bottles, or even a written list of everything you’re taking to your appointment. Your provider can help identify possible interactions, and the more they know, the safer your treatment plan will be.
Medication Guide and Dosing
Your safety also depends on how carefully you follow your prescribed treatment plan. Always read the full medication guide that comes with each prescription, even if you’ve taken the medication before. These guides are updated regularly to reflect new warnings, dosing changes, and safety notices.
Here are key tips for dosing:
- Follow your doctor’s dosing instructions exactly. Don’t self-adjust your dose to “speed up” weight loss or enhance pain relief. Doing so could increase your risk of seizures, low blood sugar, or respiratory depression.
- Take each medication at the same time each day (if instructed), and avoid combining them with high-fat meals, which can intensify side effects like nausea or blurred vision.
- If you miss a dose, don’t take two at once. Doubling up on a missed dose can lead to serious issues like stomach pain, confusion, or increased blood pressure.
- Avoid stopping either drug abruptly, especially methadone. Discontinuing without tapering may lead to opioid withdrawal, trouble sleeping, or mood disturbances.
Considering Safer Alternatives
If you’re concerned about the risks, there may be alternatives.
Your healthcare provider might recommend:
- Trying a different weight loss medication that doesn’t include naltrexone, especially if you are dependent on opioids or in recovery.
- Prioritizing non-drug approaches like a reduced-calorie diet, physical activity, and behavioral therapy.
- Adjusting methadone doses gradually if your long-term plan includes Contrave, under close supervision.
- Exploring different therapies for opioid addiction, such as buprenorphine, that may carry less risk when paired with Contrave or weight loss products.
Every treatment plan should be individualized. There’s no one-size-fits-all solution when managing chronic conditions like obesity and addiction—but there is a path that minimizes harm and maximizes benefit. It starts with open communication and informed choices.
Can You Still Use Contrave If You’re on Methadone?
It depends. In some cases, healthcare providers may cautiously prescribe Contrave to patients on methadone.
However, this requires careful monitoring, dosage adjustments, and regular checkups. Indeed, the FDA’s labeling information states that methadone and other opioid agonists or partial agonists are contraindicated for use with Contrave.
Your healthcare provider may suggest:
- Adjusting the Contrave dose or using an alternative weight loss medication
- Delaying Contrave use until methadone is tapered or discontinued
- Exploring lifestyle-based strategies such as a reduced-calorie diet and exercise
- Checking blood pressure regularly, especially if you have uncontrolled high blood pressure
- Testing blood sugar levels to prevent episodes of low blood sugar
Final Reminders
- Don’t stop or start medications without professional guidance.
- Follow your prescription label and read the medication guide closely.
- Tell your doctor about any supplements, over-the-counter drugs, or other medicines you’re taking.
- If you experience chest pain, eye pain, serious skin reactions, or dark urine, seek emergency medical attention right away.
While not everyone will experience issues from taking these two medications together, being informed—and having regular conversations with your healthcare provider—is the best way to stay safe.
Frequently Asked Questions (FAQ)
If you’re considering Contrave for weight loss while taking methadone—or vice versa—you likely have questions about potential drug interactions and safety concerns.
Below are answers to some of the most common questions patients ask. Remember, this information is not a substitute for medical advice. Always talk with your doctor or healthcare provider before making changes to your treatment plan.
1. Can you take Contrave with methadone?
In some cases, healthcare providers may prescribe Contrave and methadone together, but this combination carries significant risks and requires close medical supervision. The main concern is that naltrexone, one of the active ingredients in Contrave, can block the effects of methadone, potentially triggering opioid withdrawal symptoms.
Additionally, bupropion in Contrave may increase the risk of seizures, especially when combined with other drugs that affect the central nervous system. If you’re using methadone to manage opioid addiction or chronic pain, talk with your doctor before starting Contrave.
2. Can you take bupropion and methadone together?
While it is sometimes done under supervision, combining bupropion and methadone can raise safety concerns. Bupropion is known to lower the seizure threshold and may increase the risk of seizures, particularly in people with other risk factors like head injury, eating disorder, or use of additional CNS-active drugs. Methadone also impacts brain chemistry, which can intensify this effect.
If a healthcare provider decides to prescribe both, they will likely monitor you closely for side effects such as mood changes, trouble sleeping, or neurological symptoms. Always tell your doctor about all medications you’re taking.
3. Can you take opioids on Contrave?
No, taking opioids while on Contrave is not recommended and can be dangerous. Contrave contains naltrexone, an opioid receptor antagonist, which blocks the effects of opioids. This means opioids will be less effective or completely ineffective for pain relief or recreational use. Attempting to overcome this blocking effect by taking more opioids can lead to overdose and serious side effects, including respiratory depression and chest pain.
Always talk with your doctor if you need opioid medication for any reason while taking Contrave.
4. What medications should I avoid with Contrave?
Several other medicines can interact with Contrave and should be used cautiously or avoided altogether. These include opioids (Codeine, Oxycodone), seizure medication (Topamax), antidepressant medicine (Effexor, Lexapro), especially MAOI medications (Nardil), certain over-the-counter cold and allergy products (Benadryl), and other weight loss products (Mounjaro) or diet pills (Phentermine, Qsymia). Combining Contrave with these drugs may increase the risk of side effects such as high blood pressure, seizures, or serious skin reactions.
Also, avoid high-fat meals, which can affect how the drug is absorbed and may worsen nausea. To stay safe, tell your doctor about every medication, supplement, or herb you use, even if it seems minor.
5. What happens if you take opioids with Contrave?
Taking opioids while on Contrave can result in opioid withdrawal, which may come on suddenly and be quite severe. This happens because Contrave contains naltrexone, which blocks the opioid receptors in your brain and prevents opioids from working.
Symptoms of withdrawal may include nausea, vomiting, sweating, anxiety, stomach pain, and agitation. In some cases, it may lead to medical emergencies that require immediate medical attention.
If you’re prescribed opioid painkillers or are in recovery from opioid use, be sure to talk with your doctor before starting or continuing Contrave.
Conclusion
The combination of Contrave and methadone can be a risky combo, particularly if prescribed without full oversight. Although both drugs have unique benefits—one supporting weight loss, the other helping to treat opioid addiction—the potential for drug interactions is real and must be taken seriously.
Always work closely with your healthcare provider, especially if you’re prescribed other medicines or have underlying health conditions. Let your provider know if you experience trouble sleeping, low blood sugar, blurred vision, or suicidal thoughts. The goal is safe, effective treatment—not unexpected harm.
“Patients often assume that if medications are prescribed separately, they must be safe together,” says Dr. Olesiak. “But that’s not always the case. These two drugs can interact in unpredictable ways, and talking with your doctor is the safest way to avoid a dangerous drug interaction.”
References
FDA Contrave Labeling/Prescribing Guidelines