Mounjaro and Weight Loss Surgery: Can You Take Both?

Bariatric surgery is one of the most effective ways for individuals with severe obesity to achieve significant and sustained weight loss.
However, many patients need to lose weight before they qualify for surgery, and some may need additional support after the procedure. This raises the question: can you take Mounjaro before or after weight loss surgery?
The diabetes drug Mounjaro, with the active ingredient tirzepatide, has shown significant potential as a weight loss medication for compatible individuals. Although Mounjaro for weight loss has not yet been FDA-approved, it has been widely used off-label for this purpose.
This article will explore Mounjaro and weight loss surgery for patients, covering its benefits, risks, and medical recommendations.
Key Takeaways
- Mounjaro may be prescribed before bariatric surgery to help patients meet the weight-loss requirements for eligibility.
- After surgery, Mounjaro could assist in preventing weight regain, but its effects on altered digestion need further study.
- A licensed healthcare professional should evaluate the risks and benefits of taking Mounjaro before or after surgery based on individual health needs.
Comparison of Mounjaro and Bariatric Surgery for Weight Loss
| Factor | Mounjaro (Tirzepatide) | Bariatric Surgery |
|---|---|---|
| Mechanism of Action | GLP-1 and GIP receptor agonist that reduces appetite and regulates blood sugar. | Alters stomach size and digestion to restrict food intake and absorption. |
| Weight Loss Results | 10-20% of body weight lost over months. | Significant, often 25-35% total body weight loss. |
| FDA Approval | Approved for diabetes; prescribed off-label for weight loss. | Approved for obesity treatment. |
| Sustainability | Requires continued use to maintain weight loss. | Provides long-term results but requires lifestyle changes. |
| Pre-Surgery Use | May be prescribed to help patients meet weight-loss requirements. | Requires pre-surgery weight loss for eligibility. |
| Post-Surgery Use | May help prevent weight regain but requires medical supervision. | Patients may experience weight regain over time. |
| Medical Risks | Possible thyroid tumors, pancreatitis, kidney issues, hypoglycemia, GI distress. | Surgical risks include infections, blood clots, and digestive complications. |
| Cost & Insurance | May or may not be covered by insurance; varies by provider. | Some insurance covers surgery if the criteria are met. |
Understanding Mounjaro: How It Works for Weight Loss
Mounjaro belongs to a drug class known as GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptor agonists.
This means it mimics hormones that regulate blood sugar and appetite, leading to a decreased appetite and significant weight loss. For the best results, following a structured diet while on Mounjaro is essential. Learn more about the Mounjaro Diet and how to optimize your nutrition while taking this medication.
Clinical studies show that people lose weight on Mounjaro, making it a potential option for obese patients preparing for bariatric surgery.
Pre-Surgery Use of Mounjaro: Can It Help?
Bariatric surgery is a life-changing procedure, but it requires significant preparation. One major requirement for many patients is to lose weight before they qualify for surgery.
This may seem counterintuitive—after all, isn’t surgery meant to help with weight loss?
However, there are crucial medical reasons behind this requirement.
Why Do Patients Need to Lose Weight Before Surgery?
Surgeons and healthcare professionals often require obese patients to lose a certain percentage of their body weight before undergoing bariatric surgery for the following reasons:
- Reducing Excess Weight Lowers Surgical Risks
- Obesity increases the risk of surgical complications such as excessive bleeding, infections, and poor wound healing.
- Patients with a high body mass index (BMI) are more likely to experience complications during and after surgery.
- Losing even 5-10% of excess weight can significantly improve surgical outcomes.
- Shrinking the Liver Makes Surgery Safer
- Many obese patients have a condition called nonalcoholic fatty liver disease (NAFLD), which leads to an enlarged liver.
- A large liver can make laparoscopic bariatric surgery (the most common method) more difficult and risky.
- Losing weight before surgery helps reduce liver fat, making it easier for the surgeon to maneuver and operate safely.
- Patients Who Lose Weight Before Surgery Often Have Better Long-Term Success
- Bariatric surgery is not a quick fix—it requires a lifelong commitment to lifestyle changes.
- Patients who successfully follow a reduced-calorie diet and incorporate weight loss medications before surgery are more likely to adhere to these changes afterward.
- Losing weight pre-surgery also helps with psychological readiness, as patients begin adjusting to smaller meal portions and healthier habits.
- Meeting Insurance and Surgical Requirements
- Many insurance providers require proof that the patient has attempted weight loss through diet, exercise, or weight loss drugs before approving bariatric surgery.
- Some healthcare professionals use pre-surgery weight loss as a screening tool to ensure patients are committed to the process.
Since pre-surgery weight loss is crucial, many patients seek additional tools to help them shed pounds effectively. This is where Mounjaro may play a role.
Key Benefits and Considerations of Taking Mounjaro Before or After Bariatric Surgery
| Aspect | Pre-Surgery | Post-Surgery |
|---|---|---|
| Helps with Pre-Surgery Weight Loss | Aids in meeting weight loss criteria for surgery. | Not applicable. |
| May Prevent Weight Regain | Not applicable. | Can help maintain weight loss after surgery. |
| Affects Blood Sugar Control | Regulates blood sugar in patients with diabetes. | May cause low blood sugar, especially with dumping syndrome. |
| Potential Side Effects | GI issues, hypoglycemia, nausea, injection site reactions. | Increased risk of GI distress, altered absorption, and kidney problems. |
| Medical Supervision Required | Dosage and effects need to be monitored before surgery. | Post-surgery patients may require dosage adjustments. |
Can Mounjaro Help Patients Qualify for Surgery?
Mounjaro is a brand name for a drug called tirzepatide. It was originally developed as a diabetes drug, Mounjaro, but has gained popularity for its weight loss effects.
Although not yet FDA-approved specifically for weight loss, it is frequently prescribed off-label for this purpose.
A Mounjaro prescription may be recommended off-label for patients who need to lose weight before bariatric surgery.
It can provide multiple benefits:
- Promoting Greater Weight Loss Compared to Diet and Exercise Alone
- Clinical trials have shown that individuals lose weight on Mounjaro at significantly higher rates than with traditional methods alone.
- Some patients experience more significant weight loss of 15-20% of their body weight, which may be enough to qualify for surgery.
- Helping Regulate Blood Sugar in Patients with High Blood Pressure or High Cholesterol
- Many candidates for bariatric surgery have medical conditions such as high blood pressure, high cholesterol, or type 2 diabetes.
- Since Mounjaro belongs to the GLP-1 receptor agonist drug class, it helps regulate blood sugar, which can improve overall health and reduce risks during surgery.
- Supporting Appetite Control Through Glucose-Dependent Insulinotropic Polypeptide (GIP) Action
- Mounjaro works by mimicking glucose-dependent insulinotropic polypeptide and GLP-1 hormones, which suppress appetite.
- This results in a decreased appetite, aiding patients in sticking to a reduced-calorie diet and losing excess weight prior to surgery.
- Potentially Reducing the Need for Surgery in Some Patients
- For some individuals, taking Mounjaro may lead to more weight loss than expected, making them reconsider bariatric surgery altogether.
- In certain cases, obese patients who achieve significant weight loss with Mounjaro may no longer meet the criteria for bariatric surgery and may opt for continued medical management instead.
Precautions and Considerations
While Mounjaro offers promising benefits for weight loss and potential pre-and post-bariatric surgery support, it is not suitable for everyone.
As with any weight loss medication, a licensed healthcare professional should carefully assess whether taking Mounjaro is appropriate, considering the patient’s medical conditions, overall health, and the potential for serious side effects.
Patients should be particularly cautious of the following risks and complications:
Low Blood Sugar (Hypoglycemia)
- Mounjaro can cause low blood sugar, especially when combined with other diabetes medications such as insulin or sulfonylureas.
- Symptoms of low blood sugar include dizziness, confusion, excessive sweating, shaking, and blurred vision.
- Patients with bariatric surgery may already have altered glucose metabolism, which can increase their risk of low blood sugar episodes, particularly if they struggle with dumping syndrome (a condition where food moves too quickly from the stomach to the small intestine).
- Monitoring blood sugar levels and adjusting medication dosages accordingly is critical to avoid serious side effects related to hypoglycemia.
Kidney Problems
- Mounjaro has been associated with kidney problems, including dehydration-induced acute kidney injury.
- Bariatric surgery patients, especially those who have undergone gastric bypass, may already be at risk for dehydration due to changes in digestion and fluid absorption.
- Symptoms of kidney problems include decreased urine output, swelling in the legs or feet, and persistent nausea or vomiting.
- To minimize risk, patients should drink plenty of fluids and regularly check kidney function with their licensed healthcare professional.
Thyroid C-Cell Tumors and Thyroid Cancer Risk
- Mounjaro carries a boxed warning regarding its potential link to thyroid cancer and thyroid C-cell tumors based on animal studies.
- This means Mounjaro belongs to a class of drugs that may pose a risk for thyroid cancer, though it is not yet confirmed in humans.
- Patients with a family history of thyroid cancer, such as medullary thyroid carcinoma (MTC), or those with multiple endocrine neoplasia syndrome type 2 (MEN 2), should avoid taking Mounjaro due to the increased risk.
- Symptoms of thyroid cancer to watch for include swelling or lumps in the neck, difficulty swallowing, or changes in voice.
- If any warning signs appear, patients should consult their doctor immediately and discontinue the medication if necessary.
Serious Allergic Reactions
- Though rare, serious allergic reactions to Mounjaro can occur.
- Symptoms may include difficulty breathing, swelling of the face, lips, or tongue, and severe rash or itching.
- If a patient experiences signs of an allergic reaction, they should call their local emergency number immediately and seek urgent medical attention.
- Those with a history of severe allergies should discuss the risks with their licensed healthcare professional before starting treatment.
Other Potential Side Effects to Consider
In addition to the major risks outlined above, patients should be aware of other common side effects that could impact their ability to lose weight successfully with Mounjaro:
- Gastrointestinal Problems – Many patients report nausea, vomiting, diarrhea, or constipation, especially when first starting Mounjaro off-label for weight loss. Post-surgery patients may already have gastrointestinal problems, so these symptoms could be exacerbated.
- Injection Site Reactions – Mild pain, redness, or irritation at the upper arm or other injection sites is possible. Rotating injection locations can help minimize discomfort.
- Hair Loss – Does Mounjaro cause hair loss? Some patients have reported hair loss while taking Mounjaro. However, hair thinning is also common after bariatric surgery due to rapid weight loss and nutritional deficiencies.
- Mounjaro Increases the Risk of Pancreatitis – Though rare, Mounjaro increases the risk of pancreatitis, which can cause severe abdominal pain and nausea. Patients with a history of pancreatic disease should avoid this medication.
Importance of Medical Supervision
Since Mounjaro is prescribed off-label for weight loss, it is crucial for patients to work closely with a licensed healthcare professional to determine Mounjaro eligibility and if it is the right option.
Post-surgical patients, in particular, may require careful medication adjustments due to changes in digestion, nutrient absorption, and metabolic function.
- Electronic Prescription & Insurance Coverage – Some insurance companies may cover Mounjaro for patients preparing for bariatric surgery, but coverage varies. Patients should check with their provider regarding insurance coverage for off-label use.
- Exact Dosage Adjustments – Bariatric patients may require a low dose initially to avoid side effects. Adjustments should only be made under medical supervision.
- Long-Term Monitoring – Regular follow-ups with a healthcare professional are essential to track weight loss, ensure metabolic stability, and assess for potential complications.
While Mounjaro-lost weight can be beneficial in bariatric surgery preparation and post-op weight regain prevention, it is not without risks.
Patients should weigh the pros and cons with their licensed healthcare professional before starting to take Mounjaro.
For those who qualify, Mounjaro and weight loss surgery together may provide an effective, medically supervised approach to achieving long-term weight loss success.

Post-Surgery Use of Mounjaro: Is It Safe?
Weight Regain After Bariatric Surgery
While bariatric surgery leads to significant weight loss, some patients experience weight regain over time.
Factors such as metabolic adaptation, lifestyle choices, and medical conditions can influence long-term outcomes.
Can Mounjaro Help Maintain Weight Loss Post-Surgery?
Prescribed off-label, Mounjaro may assist in maintaining weight loss by:
- Helping people lose additional body weight in cases where surgery alone is insufficient.
- Supporting long-term appetite control to maintain weight loss.
- Managing blood sugar levels in patients with medical conditions like diabetes.
However, patients must be cautious due to the following considerations:
- Absorption Issues: After bariatric surgery, the body may absorb medications differently, affecting the exact dosage needed.
- Gastrointestinal Problems: Some post-surgery patients experience gastrointestinal problems, which could worsen with injecting Mounjaro.
- Serious Allergic Reactions: Patients should be aware of serious allergic reactions and seek emergency care if symptoms occur.
Side Effects and Risks of Mounjaro
While Mounjaro is effective, it carries potential risks, including:
- Thyroid cancer Mounjaro warning: There is a boxed warning about potential links to thyroid cancer and thyroid C-cell tumors.
- Kidney problems: Dehydration and kidney strain have been reported.
- Low blood sugar: Particularly in patients taking other diabetes medications.
- Injection site reactions: Some patients may experience redness, swelling, or irritation in the upper arm.
- Hair loss: Some individuals report hair thinning, though this is not a primary side effect.
If patients experience serious side effects, they should contact their local emergency number immediately.
Comparing Mounjaro and Bariatric Surgery
Mounjaro vs. Bariatric Surgery: How Do They Compare?
- Mounjaro’s off-label use is increasing, but it is not yet approved for weight loss like bariatric surgery.
- Bariatric surgery provides a permanent anatomical change, while Mounjaro-lost weight depends on continued medication use.
- More weight loss is typically achieved with bariatric surgery, but Mounjaro can help with weight regain.
- Patients with other health factors, like diabetes or high cholesterol, may benefit from combining both approaches under medical supervision.
Cost and Insurance Considerations
Insurance coverage varies:
- Some providers may cover Mounjaro off-label use before surgery.
- Insurance coverage for post-surgery use depends on the patient’s medical conditions.
- Online sellers may offer Mounjaro, but obtaining it through a healthcare professional is safest.
Frequently Asked Questions (FAQ)
Bariatric surgery is a significant step toward long-term weight loss and improved health.
However, patients often have questions about medication use, dietary habits, and how to optimize their results after surgery.
Below are answers to some of the most common concerns related to Mounjaro and weight loss surgery, as well as other key aspects of post-bariatric surgery care.
1. What medications should you avoid after gastric sleeve surgery?
After gastric sleeve surgery, certain medications can increase the risk of complications, including ulcers, bleeding, and irritation of the stomach lining.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil) and naproxen (Aleve), should generally be avoided, as they can cause ulcers in the smaller stomach pouch.
Extended-release medications may not be adequately absorbed due to changes in digestion, so patients should consult their licensed healthcare professional before taking them.
Additionally, some oral medications may need to be switched to liquid or chewable forms to improve absorption. Always check with your doctor before taking new medications post-surgery.
2. What is the fastest way to lose weight after bariatric surgery?
The fastest and healthiest way to lose weight after bariatric surgery is to follow a structured post-op plan. This includes eating protein-rich foods, staying hydrated, avoiding high-sugar and high-fat foods, and adhering to portion control.
Regular exercise, including walking and gradually increasing physical activity, helps maintain body weight loss.
Additionally, some patients may be prescribed weight loss medications such as Mounjaro off-label to aid in weight management.
Sticking to the recommended dietary and lifestyle changes ensures steady, sustainable weight loss while preventing complications like malnutrition or weight regain.
3. Can you take Ozempic if you have had bariatric surgery?
Yes, Ozempic (semaglutide), like Mounjaro, is a GLP-1 receptor agonist and may be prescribed off-label after bariatric surgery to help manage blood sugar levels and support additional weight loss.
However, post-surgery patients may have different medication absorption rates, which could affect the drug’s effectiveness.
Serious side effects, such as low blood sugar or gastrointestinal distress, should be closely monitored. A licensed healthcare professional should evaluate whether Ozempic is the right choice, as individual health factors, including a history of kidney problems or gastrointestinal problems, may impact safety.
4. What is the 30 rule for bariatric surgery?
The 30 rule for bariatric surgery refers to the guideline that patients should wait 30 minutes before and after eating to drink fluids.
This rule helps prevent dumping syndrome, a condition where food moves too quickly from the stomach into the intestines, leading to nausea, dizziness, and low blood sugar episodes.
Following the 30 rule also ensures that patients do not fill up on liquids instead of nutrient-dense foods. Staying hydrated is crucial, but fluids should be consumed separately from meals to maximize nutrient absorption and avoid discomfort.
5. How fast will I lose weight on Mounjaro?
How much weight a person loses on Mounjaro varies, but clinical trials have shown that most adults can experience more significant weight loss than with traditional weight loss drugs or lifestyle changes alone.
On average, patients using Mounjaro off-label for weight loss may lose 10-20% of their body weight over several months.
Factors such as medical conditions, dosage, adherence to a reduced-calorie diet, and regular physical activity influence how fast weight loss occurs.
Those combining Mounjaro with bariatric surgery should work closely with a licensed healthcare professional to track progress and adjust their treatment plan as needed.
Conclusion
For those considering bariatric surgery, taking Mounjaro before or after the procedure could offer benefits.
However, potential risks, serious side effects, and medical conditions should be discussed with a licensed healthcare professional.
While Mounjaro can aid in weight loss, its role in post-surgery management remains an evolving topic in clinical research.
Patients should work closely with their doctors to determine whether Mounjaro and weight loss surgery should be combined as part of their long-term weight loss strategy.

Is Mounjaro Safe? Risks, Side Effects, and Warnings

Mounjaro, a brand name of the generic drug tirzepatide, has gained significant attention for its role in treating type 2 diabetes and as a potential weight loss treatment.
It works by mimicking the actions of glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1), helping regulate blood sugar levels and body weight.
But is Mounjaro safe? Read on to learn about its safety, particularly in relation to side effects, serious warnings, and long-term risks.
Key Takeaways
- Mounjaro is FDA-approved for treating type 2 diabetes and is being studied for weight loss. However, it carries important safety warnings, particularly regarding thyroid tumors and severe allergic reactions.
- Side effects of Mounjaro include stomach pain, nausea, and low blood sugar, with more severe risks like kidney problems and gallbladder issues requiring medical attention.
- People with a personal or family history of thyroid cancer or certain other medical conditions should discuss potential risks with their healthcare professionals before taking Mounjaro.
How Mounjaro Works
Mounjaro belongs to a drug class known as dual GIP and GLP-1 receptor agonists. It stimulates insulin release while also reducing glucagon secretion, leading to lower blood sugar levels.
Additionally, Mounjaro affects appetite by slowing gastric emptying, contributing to decreased appetite and subsequent weight loss for compatible individuals.
Clinical trials have shown that taking Mounjaro helps improve blood sugar control and supports significant reductions in body weight.
Understanding the Role of Glucose-Dependent Insulinotropic Polypeptide (GIP) in Mounjaro’s Function
Mounjaro’s efficacy in blood sugar control and weight loss is primarily due to its unique mechanism of action, which targets both glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptors. This dual action differentiates Mounjaro from other diabetes medications that target only GLP-1 receptors.
Research on GIP’s role in metabolism, insulin release, and appetite regulation suggests that its combined activation with GLP-1 may contribute to Mounjaro’s effects on blood sugar control and weight management.
How GLP-1 and GIP Work Together for Better Blood Sugar Control
GLP-1 receptor agonists, such as Ozempic and Wegovy, primarily stimulate insulin secretion and reduce glucagon levels after meals, helping regulate blood sugar.
While this mechanism is effective, Mounjaro takes it a step further by also activating GIP receptors, leading to additional metabolic benefits.
The combination of GLP-1 and GIP receptors enhances blood sugar control by:
- Increasing insulin secretion in response to food intake, preventing post-meal blood sugar spikes.
- Suppressing glucagon release, reducing excess glucose production by the liver.
- Improving insulin sensitivity, helping the body use insulin more effectively.
Clinical trials have shown that this dual-action approach results in more significant reductions in blood sugar levels compared to GLP-1-only drugs, making Mounjaro a promising option for individuals struggling to achieve glycemic control with other diabetes treatments.
But does Mounjaro help with weight loss?
The Role of GIP in Metabolism, Insulin Release, and Appetite Suppression
GIP, a hormone naturally produced in the small intestine, plays a key role in metabolic regulation, insulin production, and fat storage.
While GLP-1 primarily affects insulin secretion and slows digestion, GIP provides additional benefits that contribute to Mounjaro’s efficacy.
Key functions of GIP include:
- Enhancing insulin release from pancreatic beta cells in response to food, particularly carbohydrates.
- Regulating fat metabolism by influencing how the body stores and breaks down fat.
- Suppressing appetite by acting on the brain’s hunger centers, reducing food intake.
Unlike GLP-1, which primarily reduces appetite and slows gastric emptying, GIP plays a broader role in metabolism, helping the body more effectively store and utilize energy.
This may explain why Mounjaro leads to more significant weight loss compared to other GLP-1-based medications.
Mounjaro Safety Overview
| Category | Details |
|---|---|
| FDA Approval | Approved for type 2 diabetes; potential approval for weight loss under review. |
| Primary Use | Blood sugar regulation and weight management. |
| Mechanism of Action | Dual action on GLP-1 and GIP receptors, enhancing insulin secretion and appetite suppression. |
| Key Benefits | Improves blood sugar control, supports weight loss, and increases insulin sensitivity. |
| Common Side Effects | Nausea, vomiting, diarrhea, stomach pain, decreased appetite. |
| Serious Risks | Thyroid cancer risk, kidney problems, gallbladder issues, severe allergic reactions, stomach paralysis. |
| Who Should Avoid | Individuals with a personal or family history of thyroid cancer, severe kidney disease, multiple endocrine neoplasia syndrome type 2 (MEN 2). |
| Drug Interactions | May interact with other diabetes medications, birth control pills, and alcohol. |
| Long-Term Safety Concerns | Long-term effects still under study, including thyroid cancer risk and metabolic impact. |
How Mounjaro Differs From GLP-1-Only Drugs
Traditional GLP-1 receptor agonists like Ozempic, Rybelsus, and Wegovy are effective for blood sugar control and weight management but do not engage GIP receptors, which play a role in metabolism and insulin regulation.
The inclusion of GIP activation in Mounjaro has been associated with:
- Enhanced insulin secretion in response to meals, contributing to improved glucose regulation.
- Increased appetite suppression, which may support greater weight reduction.
- Potential effects on fat metabolism that could influence long-term weight management.
Because of this dual mechanism, Mounjaro compares favorably to GLP-1-based treatments in both diabetes management and weight loss outcomes.
It is particularly beneficial for individuals who require a more potent blood sugar-lowering effect or those seeking more significant weight reduction without increasing the severity of side effects seen with high-dose GLP-1 agonists.
The Future of Dual-Action Diabetes and Weight Loss Treatments
Mounjaro is part of a newer class of diabetes treatments that incorporates both GLP-1 and GIP receptor activation, expanding beyond the mechanisms of GLP-1-only medications. This dual approach may provide broader metabolic effects, making it a potential option for managing both type 2 diabetes and obesity.
Ongoing research may lead to the development of additional dual-hormone treatments, further expanding therapeutic options for individuals seeking improved blood sugar regulation and weight management.
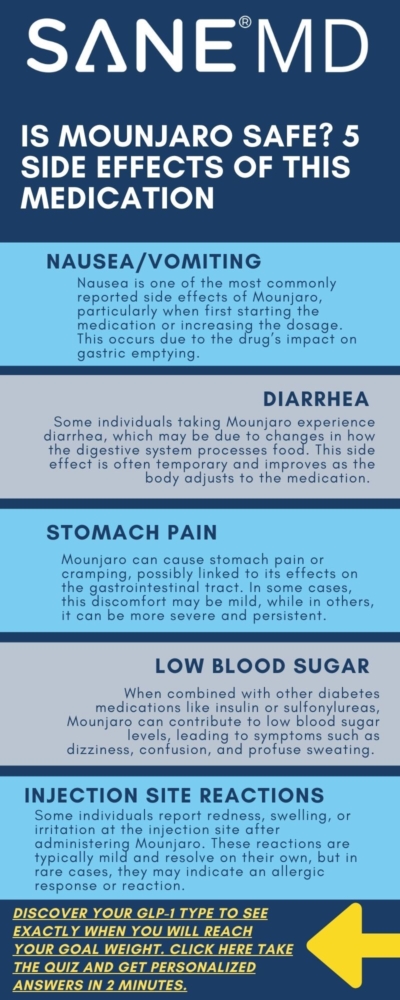
Side Effects of Mounjaro
The side effects of Mounjaro can range from mild digestive discomfort to more severe medical complications. Common side effects include nausea, vomiting, diarrhea, and abdominal pain.
Clinical trials suggest that these effects are most pronounced during the first few weeks of treatment as the body adjusts to the drug.
1. Gastrointestinal Issues
Stomach paralysis, also called gastroparesis, has been reported in some individuals taking Mounjaro. This condition leads to symptoms such as severe nausea, vomiting, and bloating.
Stomach pain and injection site reactions are also possible side effects, particularly when adjusting to new Mounjaro doses.
2. Thyroid Cancer Risk
One of the most serious warnings associated with Mounjaro is the increased risk of thyroid tumors, including thyroid cancer. Animal studies suggest a potential link, but more research is needed to confirm the risk in humans. People with a family history of thyroid cancer should avoid using Mounjaro.
The FDA requires a black box warning about thyroid tumors, making this a critical factor for those considering a Mounjaro prescription.
3. Blood Sugar Effects
Since Mounjaro is used to treat diabetes, it plays a role in managing blood sugar levels. However, it can sometimes lower blood sugar too much, leading to hypoglycemia. Low blood sugar can cause dizziness, confusion, and fainting, especially when combined with other diabetes medications.
Monitoring blood sugar is crucial for anyone taking Mounjaro, particularly if they are using other diabetes treatments.
4. Kidney and Gallbladder Problems
Mounjaro can contribute to dehydration, which may lead to kidney problems or worsen existing kidney disease. Gallbladder problems, such as gallstones, have also been reported in clinical trials.
Symptoms like severe pain in the upper abdomen or persistent nausea may indicate gallbladder issues that require medical attention.
5. Allergic Reactions
Some individuals may experience a serious allergic reaction to Mounjaro, which can manifest as rash, swelling, or difficulty breathing. A severe allergic reaction requires immediate medical attention, as it may progress to anaphylaxis.
Injection site reactions, including redness and irritation, are also possible but typically mild.
Mounjaro for Weight Loss
Although Mounjaro is primarily prescribed for diabetes management, clinical trials have demonstrated significant weight loss effects. Its mechanism, which includes appetite suppression and delayed gastric emptying, has been associated with reductions in body weight.
While Mounjaro has shown promising results compared to other weight loss medications, its approval for weight management is still under review. However, some patients are already exploring its potential role in bariatric surgery. Our article, “Mounjaro and Weight Loss Surgery: Can You Take Both?” explores whether it can be used before or after surgery, along with its benefits and risks.

Drug Interactions and Safety Considerations
Interaction With Other Diabetes Medications
Mounjaro can interact with other diabetes medications, including insulin, increasing the risk of low blood sugar.
People taking Mounjaro should work closely with healthcare professionals to adjust their diabetes treatments accordingly.
Birth Control Pills and Other Drugs
Taking Mounjaro may reduce the effectiveness of birth control pills due to delayed gastric emptying. Alternative contraceptive methods should be considered to prevent unintended pregnancy.
Drug interactions with Mounjaro should be discussed with a healthcare provider, particularly when taking other drugs that affect blood sugar levels or kidney function.
Drinking Alcohol and Mounjaro
Drinking alcohol while taking Mounjaro can further impact blood sugar regulation, potentially leading to high blood sugar levels or severe hypoglycemia.
Those who consume alcohol should do so cautiously and monitor their blood sugar levels closely.
Dosage, Administration, and Storage
Mounjaro doses are typically started at a lower amount and gradually increased to minimize side effects. The maximum dosage depends on individual needs and medical conditions. People inject Mounjaro under the skin, often in the upper arm, thigh, or abdomen.
If a missed dose occurs, the next dose should be taken as soon as possible unless it is close to the next scheduled injection.
To store Mounjaro properly, it should be kept in the refrigerator but can remain at room temperature for a limited period if necessary.
Mounjaro and Long-Term Use: What We Know So Far
As Mounjaro continues to gain popularity for blood sugar control and weight loss, questions about its long-term safety remain.
While clinical trials have demonstrated strong efficacy in the short term, ongoing research is needed to determine its effects over years or decades of use.
Potential Risks Associated With Prolonged Use
Prolonged use of Mounjaro may lead to gastrointestinal issues, such as persistent nausea, stomach pain, or stomach paralysis. Additionally, its effects on the pancreas, cardiovascular health, and metabolism over extended periods are still being studied.
Patients taking Mounjaro for years should have regular check-ups to monitor for any emerging complications.
Long-Term Risks: Thyroid Cancer and Kidney Disease Concerns
One of the most serious warnings associated with Mounjaro is its potential link to thyroid tumors, including thyroid cancer. While this risk has been observed in animal studies, human data is still limited.
Those with a family history of thyroid cancer should discuss these concerns with their doctor before taking Mounjaro long-term.
Additionally, some patients have reported kidney problems, particularly if they experience severe dehydration from persistent nausea or vomiting.
Individuals with pre-existing kidney disease should be closely monitored while using Mounjaro to reduce the risk of further complications.
Considerations for Long-Term Users
For individuals needing to take Mounjaro for years, healthcare professionals must balance benefits versus potential risks.
Long-term use may be necessary for maintaining weight loss and blood sugar control, but patients should undergo regular screenings for thyroid abnormalities, kidney function, and other potential side effects.
Adjustments to dosage or switching to other treatments may be required based on individual tolerance and health changes over time.
When to Seek Medical Help
Some side effects of Mounjaro may require immediate medical attention. Severe abdominal pain, symptoms associated with thyroid cancer, and warning signs of a medical emergency—such as difficulty breathing due to a severe allergic reaction—should be promptly evaluated by a healthcare professional.
Those with a personal or family history of thyroid cancer or kidney disease should consult their doctor before taking Mounjaro.
Frequently Asked Questions (FAQ) About Mounjaro
Mounjaro has been studied for its role in regulating blood sugar levels and supporting weight management.
However, many people have questions about what Mounjaro is used for, its safety, who should take it, and its long-term effects.
Below are answers to some of the most common questions about Mounjaro.
1. What are the cons of taking Mounjaro?
While Mounjaro is highly effective for blood sugar control and weight loss, it comes with potential downsides. Common side effects of Mounjaro include nausea, vomiting, diarrhea, stomach discomfort, and a reduced appetite.More serious risks include low blood sugar, kidney problems, gallbladder issues, and an increased risk of thyroid tumors.
Additionally, some patients experience stomach paralysis, which can lead to severe digestive issues. Patients taking Mounjaro should be closely monitored by their healthcare provider to manage these potential risks.
2. What does Mounjaro do to your body?
Mounjaro works by activating two hormone receptors, GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). These hormones help regulate insulin release, glucose metabolism, and appetite control. As a result, Mounjaro helps lower blood sugar levels, suppress appetite, and slow down digestion, leading to weight loss for compatible individuals and better metabolic health.
However, due to its effect on the gastrointestinal system, it can also cause side effects such as nausea, stomach discomfort, and digestive issues.
3. Who should not take Mounjaro?
Mounjaro is not recommended for individuals with:
- A personal or family history of medullary thyroid cancer.
- A history of multiple endocrine neoplasia syndrome type 2 (MEN 2).
- Severe kidney disease or a history of kidney failure.
- A history of serious allergic reactions to tirzepatide or any of its ingredients.
- Pregnant or breastfeeding women should consult a doctor before taking Mounjaro, as its effects on pregnancy are not well-studied.
Additionally, people with severe gastrointestinal disorders, such as gastroparesis (stomach paralysis), may not tolerate Mounjaro well due to its effect on digestion.
4. Is Mounjaro safe for people without diabetes?
Mounjaro is currently FDA-approved for treating type 2 diabetes, but it has also shown significant benefits for weight loss in non-diabetic individuals. Clinical trials suggest that Mounjaro helps reduce body weight even in those without diabetes.
However, since it affects blood sugar levels, it may cause low blood sugar or other metabolic changes in non-diabetic users. Anyone considering taking Mounjaro for weight loss should consult their doctor to evaluate potential risks and benefits.
5. Is Mounjaro approved for weight loss?
Mounjaro is currently not FDA-approved for weight loss, but clinical trials suggest it may be a highly effective option for weight management in a subset of individuals. Patients using Mounjaro for diabetes have reported significant weight loss, and ongoing research is evaluating its potential for approval as a dedicated weight loss treatment.
Given its success in clinical trials, it is expected that Mounjaro will receive FDA approval for weight loss in the near future.
Conclusion
Mounjaro is FDA-approved for diabetes management and is being explored for weight loss treatment. However, individuals considering taking Mounjaro should be aware of potential risks, including thyroid tumors, stomach paralysis, and allergic reactions.
Those with pre-existing medical conditions should discuss safety concerns with their healthcare professionals. Monitoring blood sugar levels, understanding potential drug interactions, and recognizing serious side effects are crucial steps in ensuring the safe use of Mounjaro.

Contrave and Melatonin Drug Interactions: Is It Safe?
If you’ve been wondering what Contrave is used for and whether there are any drug interactions, you’ve come to the right place.
Contrave, a prescription medication containing naltrexone bupropion, is commonly used for chronic weight management in certain individuals with a high initial body mass index. However, questions often arise regarding the prevalence of Contrave drug interactions, including melatonin.
Understanding potential drug interactions, systemic exposure, and associated risk factors is essential before combining these substances.
This article provides an objective and comprehensive analysis of Contrave and melatonin drug interactions, including possible side effects on blood pressure, the risk of seizures, and other potential concerns.
Key Takeaways
- Taking Contrave with melatonin may increase the risk of adverse reactions, including high blood pressure and central nervous system (CNS) toxicity.
- Contrave treatment affects the seizure threshold, which may be further impacted by melatonin’s sedative effects, leading to an increased risk of seizures.
- Individuals with psychiatric disorders, bipolar disorder, or major depressive disorder should consult a licensed healthcare professional before taking Contrave and melatonin together.
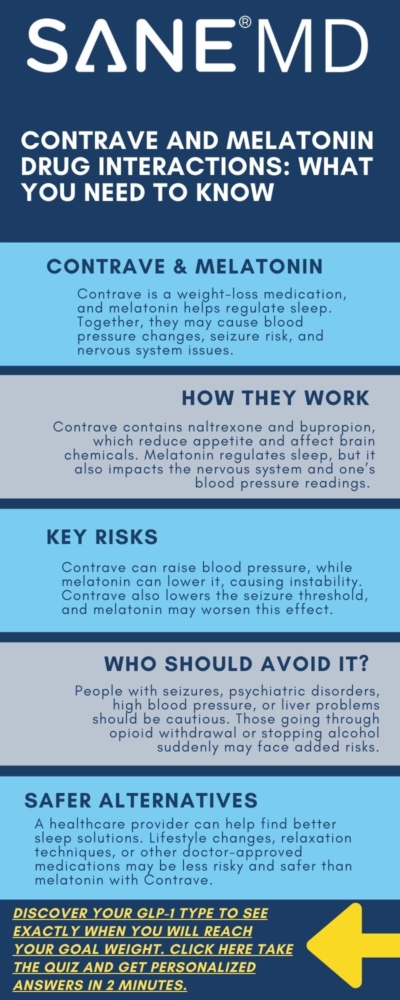
Understanding Contrave and Melatonin
Contrave is a prescription medication designed for chronic weight management in compatible adults with obesity or overweight individuals with weight-related health conditions. It combines two active ingredients: naltrexone hydrochloride and bupropion hydrochloride (bupropion HCL).
This drug is part of a broader treatment regimen that includes a reduced-calorie diet and increased physical activity to help patients achieve clinically meaningful weight loss.
However, the effects of Contrave interactions with other substances, including melatonin, remain a critical concern for safety and efficacy.
Melatonin is a widely used over-the-counter supplement that helps regulate sleep cycles. While it is generally considered safe, taking Contrave alongside melatonin may increase the risk of certain complications, such as high blood pressure, CNS toxicity, and seizure threshold alterations.
Because Contrave has known effects on blood pressure, cardiovascular health, and neurological function, adding melatonin to the regimen requires careful consideration.
Mechanism of Action
Understanding how Contrave and melatonin work individually can provide insight into the potential risks when taken together.
Naltrexone Hydrochloride
Naltrexone hydrochloride is commonly used to manage opioid dependence and opioid withdrawal. It functions by blocking opioid receptors in the brain, which can reduce cravings and suppress appetite. This mechanism plays a crucial role in Contrave treatment, particularly for certain individuals who struggle with food cravings and compulsive eating behaviors.
However, naltrexone hydrochloride may increase the risk of adverse reactions when combined with other substances that affect the central nervous system.
Bupropion Hydrochloride (Bupropion HCL)
Bupropion hydrochloride is an antidepressant drug originally developed to treat depression and later approved to aid in smoking cessation and weight loss. It works by inhibiting the reuptake of dopamine and norepinephrine, enhancing mood and energy levels while also reducing appetite.
However, bupropion hydrochloride can lower the seizure threshold, meaning that individuals taking Contrave already have an increased risk of seizures.
Melatonin
Melatonin is a naturally occurring hormone produced by the pineal gland that regulates sleep-wake cycles. It is frequently used as a sleep aid, particularly for individuals with insomnia, jet lag, or other sleep disorders. While melatonin is generally well-tolerated, it may interact with Contrave by affecting systemic exposure to its active components. Additionally, melatonin can influence blood pressure, further complicating the cardiovascular risks associated with Contrave.
When combining Contrave and melatonin, patients should consult a healthcare provider to evaluate potential risks and determine whether a dosage adjustment is necessary to prevent adverse effects.
Contrave and Melatonin Drug Interactions Chart
| Category | Contrave | Melatonin |
|---|---|---|
| Drug Combination | Naltrexone Hydrochloride + Bupropion Hydrochloride | Natural sleep-regulating hormone |
| Primary Use | Chronic weight management | Regulates sleep cycles and aids in treating insomnia |
| Potential Interactions | Interacts with melatonin, opioids, antidepressants, and other CNS-affecting drugs | Affects systemic exposure of Contrave and neurotransmitter function |
| Effects on Blood Pressure | Can increase blood pressure, particularly in individuals with hypertension | May lower blood pressure, leading to unpredictable cardiovascular effects |
| Effects on CNS | Lowers seizure threshold, increasing seizure risk | Can influence neurotransmitter activity, potentially causing drowsiness or mood instability |
| Who Should Avoid? | Individuals with seizure disorder, severe hepatic impairment, psychiatric disorders, or opioid dependence | Those with psychiatric disorders, blood pressure issues, or those taking CNS-affecting drugs |
| Additional Risks | May increase the risk of suicidal thoughts, hypertensive reactions, and CNS toxicity | May cause excessive drowsiness, confusion, and worsen CNS toxicity when combined with Contrave |
| Precautions | Avoid alcohol, high-fat meals, and other CNS stimulants or depressants | Consult a healthcare provider before use, especially when taking other medications |
Contrave and Melatonin Drug Interactions
It’s crucial to consider Contrave side effects and safety considerations for weight loss, which includes examining potentially negative drug interactions.
When considering certain drug interactions, it is essential to evaluate how Contrave and melatonin might impact various health conditions, particularly those related to blood pressure, neurological function, and overall cardiovascular morbidity. Because both drugs influence different biological processes, their combination may introduce unpredictable physiological effects, some of which may increase the risk of adverse health outcomes.
Additionally, Contrave treatment affects neurotransmitters and cardiovascular function, while melatonin plays a role in sleep regulation and vascular control. The simultaneous use of these two substances may interact with Contrave’s active metabolite, altering systemic exposure and potentially leading to undesirable effects.
Effects on Blood Pressure and Cardiovascular Health
One of the primary concerns when taking Contrave is its impact on blood pressure. Contrave interactions with other drugs that affect vascular function can lead to hypertensive reactions or fluctuations in high blood pressure levels.
This is particularly relevant for individuals with preexisting cardiovascular conditions, as Contrave treatment may increase the risk of severely high blood pressure, putting patients at greater risk for cardiovascular morbidity.
Melatonin, on the other hand, has been observed to have a mild blood pressure-lowering effect in some individuals, particularly those with hypertension. However, its impact is not entirely predictable, as research suggests it can sometimes result in opposite effects, depending on dosage, timing, and an individual’s baseline cardiovascular health.
When Contrave and melatonin are taken together, these opposing mechanisms can potentially result in unpredictable blood pressure fluctuations—either dangerously high or abnormally low. Such instability in cardiovascular regulation may lead to dizziness, fainting, or increased cardiovascular stress.
Therefore, it is highly recommended that patients with high blood pressure, hypertensive reactions, or other cardiovascular conditions consult a healthcare provider before combining Contrave with melatonin. Close monitoring may be necessary to determine whether a dosage adjustment is required to maintain stable blood pressure levels and avoid adverse effects.
It’s important to note that if taking Contrave and Prozac together, drug interactions that affect blood pressure and cardiovascular health can also occur.
Risk of Seizures and CNS Toxicity
Another significant concern when taking Contrave alongside melatonin is the increased risk of seizures and central nervous system (CNS) toxicity.
Contrave contains bupropion hydrochloride, which is known to lower the seizure threshold, meaning it makes seizures more likely to occur, especially in individuals with seizure disorders or neurological vulnerabilities.
This risk is even higher in patients who:
- Have a history of seizure disorder or bipolar disorder
- Are undergoing opioid withdrawal
- Have severe hepatic impairment, which affects drug metabolism
- Suddenly stop drinking alcohol, which can increase the risk of withdrawal seizures
Melatonin, though primarily a sleep-regulating hormone, also exerts neurological effects by interacting with neurotransmitter systems. In some individuals, particularly those with preexisting neurological conditions, melatonin may contribute to CNS toxicity, leading to symptoms such as:
- Increased drowsiness and confusion
- Dizziness and balance issues
- Exacerbation of bipolar disorder or psychiatric disorders
When used in combination, Contrave and melatonin may increase the risk of these CNS-related side effects, particularly for individuals who already have neurological or psychiatric conditions. Additionally, the active metabolite of Contrave could further influence melatonin metabolism, leading to unpredictable drug interactions and possible adverse effects.
For individuals who are at risk for seizures, CNS toxicity, or psychiatric complications, it is strongly advised to seek guidance from a healthcare provider before combining these two substances. A licensed healthcare professional can determine whether a dosage adjustment or alternative treatment approach is necessary to mitigate potential risks.
Additional Risk Factors and Contraindications
When considering Contrave treatment, it is essential to assess individual risk factors that may increase the risk of serious adverse reactions. Certain health conditions, medications, and lifestyle factors can make Contrave interactions with melatonin and other drugs more dangerous.
Individuals with specific medical histories should avoid combining Contrave and melatonin or consult a licensed healthcare professional to determine whether a dosage adjustment is necessary.
Prescription Drugs, Over-the-Counter Medications, and Other Drugs
The potential for Contrave interactions extends far beyond melatonin. Other drugs, including prescription drugs and over-the-counter drugs, may also increase the risk of dangerous side effects when combined with Contrave treatment.
Patients should inform their healthcare provider about all medications they are taking, including:
- Monoamine oxidase inhibitors (MAOIs) – These medications, often used to treat depression and Parkinson’s disease, can cause severe hypertensive reactions when combined with Contrave.
- Antiepileptic drugs – Used to control seizures, these medications may be affected by Contrave’s ability to lower the seizure threshold, potentially leading to an increased risk of seizures.
- Other drugs that affect neurotransmitters – This includes antidepressant drugs like Wellbutrin SR, as well as medications used for bipolar depression and psychiatric disorders.
- Over-the-counter drugs that affect blood pressure – Common decongestants and certain pain relievers may further contribute to high blood pressure and hypertensive reactions.
Healthcare professionals may need to recommend a dosage adjustment or suggest alternative treatments to avoid clinically significant drug interactions.
Alcohol Consumption and Withdrawal
Drinking alcohol while on Contrave is strongly discouraged, as it may increase the risk of seizures and CNS toxicity.
Alcohol can also interfere with Contrave’s effects on neurotransmitter activity, leading to unpredictable psychological and physiological responses.
Patients should be aware that Contrave treatment may increase the risk of adverse reactions if alcohol is consumed, including:
- Sudden spikes in blood pressure
- Increased dizziness, drowsiness, or impaired coordination
- Heightened risk of seizures, especially in patients with preexisting neurological conditions
- Greater CNS toxicity, leading to confusion, agitation, or mood disturbances
Additionally, those who suddenly stop drinking alcohol may experience withdrawal symptoms, which could further interact with Contrave in dangerous ways. Alcohol withdrawal symptoms, such as seizures, tremors, and anxiety, may be worsened by Contrave’s effects on neurotransmitters.
To ensure safe Contrave treatment, individuals who drink alcohol should:
- Consult a healthcare provider before starting or stopping alcohol use
- Gradually taper alcohol consumption to avoid withdrawal complications
- Avoid excessive alcohol intake, particularly when also taking melatonin or other CNS-affecting drugs
By managing alcohol use, medication interactions, and individual risk factors, patients can reduce the increased risk of dangerous adverse effects associated with Contrave treatment.
FAQ: Contrave and Melatonin Drug Interactions
1. What medications should not be taken with Contrave?
Contrave interacts with several medications that can either increase the risk of serious side effects or reduce its effectiveness.
The following medications should generally be avoided or used with extreme caution under a healthcare provider’s supervision:
- Monoamine Oxidase Inhibitors (MAOIs): Combining Contrave with MAOIs (e.g., phenelzine, tranylcypromine) can cause severe hypertensive reactions and dangerous neurotransmitter imbalances.
- Antiepileptic drugs: Medications like carbamazepine, phenytoin, and valproate can further lower the seizure threshold, increasing the risk of seizures.
- Opioid-based medications: Since naltrexone hydrochloride is an opioid antagonist, Contrave should not be taken with opioids like morphine, oxycodone, or hydrocodone, as it may trigger opioid withdrawal symptoms.
- Antidepressant drugs (Wellbutrin SR, SSRIs, SNRIs): Combining Contrave with other bupropion-containing medications or antidepressants may increase the risk of suicidal thoughts and behaviors or serotonin syndrome.
- Over-the-counter decongestants: Certain OTC cold and flu medications containing pseudoephedrine or phenylephrine can increase blood pressure, compounding Contrave’s cardiovascular effects.
Patients must always inform their healthcare provider about any prescription medications, over-the-counter drugs, or herbal supplements they are using to prevent clinically significant drug interactions.
2. Can I take melatonin while on BuPROPion?
Although melatonin is widely used as a natural sleep aid, taking it with bupropion hydrochloride, one of the active ingredients in Contrave, may lead to unpredictable effects on the central nervous system.
Bupropion lowers the seizure threshold, meaning it makes seizures more likely to occur, particularly in individuals with a history of neurological conditions or seizure disorders. Because melatonin also influences neurotransmitter activity, combining it with bupropion could increase the risk of seizures and other adverse neurological effects.
Additionally, melatonin’s sedative properties may counteract bupropion’s stimulating effects, potentially leading to disrupted sleep patterns or mood instability.
3. Does Contrave make it hard to sleep?
Contrave may cause sleep disturbances, including insomnia and vivid dreams. These effects are primarily due to bupropion hydrochloride, which has stimulant-like properties that can increase alertness and interfere with normal sleep patterns.
Some patients find it difficult to fall asleep or stay asleep, while others report feeling more restless at night. The impact on sleep can be particularly pronounced if Contrave is taken too late in the day.
To reduce sleep disruptions, it is generally recommended to take Contrave in the morning.
4. What drugs do not interact well with melatonin?
Although melatonin is often considered a safe supplement, it can interact with various medications, leading to unintended side effects. Blood pressure medications, including beta-blockers and calcium channel blockers, may have altered effectiveness when taken with melatonin, potentially causing unpredictable blood pressure fluctuations.
Antidepressants, such as SSRIs and SNRIs, may interact with melatonin in a way that exacerbates depression or causes mood instability. Individuals taking antiepileptic drugs should also use caution, as melatonin may interfere with neurological stability and increase the risk of seizures.
It is essential to consult a healthcare provider before combining melatonin with any prescription medication.
5. What to avoid while on Contrave?
There are several substances and behaviors that should be avoided while taking Contrave to prevent complications and maximize its effectiveness. Drinking alcohol is strongly discouraged, as Contrave lowers the seizure threshold, and alcohol consumption can significantly increase the risk of seizures and central nervous system toxicity.
Individuals who suddenly stop drinking alcohol while on Contrave may experience withdrawal symptoms, which could further interact with the medication’s effects on neurotransmitters. High-fat meals should also be avoided, as they may increase systemic exposure to Contrave’s active components, leading to a higher likelihood of experiencing adverse reactions.
Conclusion
Taking Contrave with melatonin may increase the risk of blood pressure fluctuations, seizures, and CNS toxicity. Individuals with psychiatric disorders, seizure disorders, or other health conditions should consult a licensed healthcare professional before combining these substances.
To minimize risks, patients should disclose all medications, including over-the-counter drugs, and adhere to their prescribed treatment regimen. If any adverse effects occur, immediate medical consultation is necessary.