Contrave and Alcohol Drug Interactions: Dangers & Risks
Contrave is a prescription medication designed to aid weight loss in certain adults by combining two active drugs: naltrexone and bupropion. While it can be effective in supporting weight management, taking Contrave comes with potential risks, especially when combined with alcohol use.
Contrave and alcohol drug interactions can lead to severe complications, increasing the risk of side effects, impacting mental health, and causing significant changes in blood pressure. Patients should be aware of these possible Contrave drug interactions to avoid dangerous health consequences.
Key Takeaways
- Increased Risk of Adverse Effects: Drinking alcohol while taking Contrave can increase the risk of seizures, mental health changes, and fluctuations in blood pressure.
- Severe Cardiovascular and Neurological Concerns: The combination of alcohol and Contrave may contribute to irregular heartbeat, high blood pressure, and a higher likelihood of experiencing seizures.
- Healthcare Provider Consultation is Essential: Patients should consult their healthcare provider before consuming alcohol while on Contrave treatment to assess their individual risk factors and potential complications.
Understanding Contrave and Alcohol Drug Interactions
Contrave is a combination drug used to aid weight management in certain adults. It consists of two active ingredients: naltrexone, an opioid antagonist, and bupropion, an antidepressant that helps treat depression and supports smoking cessation.
But what does Contrave do when combined with alcohol? While this formulation can be effective in supporting weight loss for compatible individuals, drinking alcohol while taking Contrave introduces serious risks. Alcohol can alter the drug effects of Contrave, leading to dangerous interactions that impact physical and mental health.
The Science Behind Alcohol’s Effects on the Body
Neurotransmitter Disruption
Alcohol affects neurotransmitters in the brain, primarily enhancing the effects of gamma-aminobutyric acid (GABA), which induces relaxation, and inhibiting glutamate, which leads to slowed brain activity. These effects can cause drowsiness, impaired motor skills, and mood swings.
When alcohol is combined with Contrave, which also affects neurotransmitter activity, the result can be extreme mood swings, heightened anxiety, or increased drowsiness, making daily tasks and decision-making more difficult.
It can also increase the risk of seizures. As mentioned above, alcohol impacts the brain’s electrical activity and neurotransmitter balance. When combined with Contrave, which already has stimulant-like effects due to bupropion, the risk of abnormal brain activity leading to seizures becomes significantly higher.
Additionally, if a person with a seizure disorder suddenly stops drinking alcohol while on Contrave, withdrawal symptoms can trigger seizures, even in individuals who have never experienced one before.
Metabolic Impact
The liver is responsible for metabolizing both alcohol and Contrave, which means excessive alcohol consumption can interfere with the breakdown of the drug. This can lead to intensified or unpredictable drug effects, increasing the risk of toxicity.
Additionally, alcohol can alter the body’s metabolic rate, potentially reducing the effectiveness of Contrave in weight loss treatment by impairing fat metabolism and promoting fat storage instead.
Cardiovascular Effects
Alcohol consumption can have varying effects on blood pressure, sometimes causing a dangerous drop or an unexpected spike. For individuals taking Contrave, which already carries a risk of fluctuating blood pressure, this interaction can be particularly dangerous.
Chronic alcohol consumption can also weaken the heart muscle, increasing the likelihood of long-term cardiovascular complications when combined with Contrave treatment.
Contrave and Alcohol Drug Interactions: Risks and Explanations
| Risk/Concern | Explanation |
|---|---|
| Increased Risk of Seizures | Alcohol lowers the seizure threshold, and Contrave contains bupropion, which can increase seizure risk. The combination makes seizures more likely, especially in those with a history of seizure disorder. |
| Fluctuations in Blood Pressure | Both Contrave and alcohol can cause sudden changes in blood pressure, resulting in dangerously high or low blood pressure, increasing cardiovascular risks such as heart attack or stroke. |
| Mental Health Risks | Alcohol is a depressant that can counteract the mood-regulating effects of Contrave, leading to worsened depression, anxiety, mood swings, or even suicidal thoughts. |
| Impaired Judgment | Alcohol reduces inhibitions and decision-making abilities. Drinking while on Contrave may lead to overeating, engaging in risky behaviors, or neglecting weight loss goals. |
| Low Blood Sugar | Alcohol interferes with glucose metabolism, increasing the risk of hypoglycemia (low blood sugar), particularly dangerous for individuals with diabetes or metabolic disorders. |
| Liver Strain and Toxicity | Both Contrave and alcohol are processed in the liver. Consuming alcohol while on Contrave can increase the risk of liver damage or impaired drug metabolism. |
| Binge-Eating Episodes | Contrave is designed to suppress appetite, but alcohol lowers self-control and increases hunger, which may lead to unplanned binge eating and hinder weight loss progress. |
| Gastrointestinal Discomfort | Alcohol can irritate the digestive system, worsening nausea, acid reflux, and ulcers, which are potential side effects of Contrave. |
| Potential Drug Interactions | Contrave interacts with various medications, including opioids, antidepressants, blood pressure drugs, and diabetes medications. Alcohol can exacerbate these interactions and increase health risks. |
| Consult a Healthcare Provider | Patients should consult their healthcare provider before consuming alcohol while taking Contrave to assess their individual risk factors and prevent serious complications. |
Long-Term Health Risks of Mixing Contrave and Alcohol
Cardiovascular Damage
Long-term alcohol use, combined with Contrave, can contribute to serious cardiovascular complications, including hypertension, stroke, and heart attack. Alcohol can raise blood pressure levels, which may further increase the risk of severely high blood pressure in individuals taking Contrave.
Over time, this strain on the cardiovascular system can lead to heart failure or other serious health conditions.
Low Blood Sugar
One of the critical risks associated with combining Contrave and alcohol is the potential for low blood sugar (hypoglycemia), particularly in individuals with diabetes or those prone to blood sugar fluctuations.
Contrave influences metabolism and appetite regulation, which can affect blood sugar levels, while alcohol further complicates this balance by altering how the body processes glucose.
Mental Health Decline
Bupropion, one of Contrave’s active ingredients, is used to treat depression, meaning any additional depressant effects from alcohol can negatively impact mental health. Individuals with pre-existing depression or anxiety may find that alcohol worsens their condition, leading to increased feelings of hopelessness, panic attacks, or even suicidal thoughts.
Because Contrave affects the brain’s chemistry, drinking alcohol while taking it can intensify these risks.
Metabolic and Liver Complications
Since both alcohol and Contrave are processed in the liver, their combined use may lead to liver damage. The liver’s reduced ability to efficiently metabolize medications can increase the risk of drug accumulation, leading to intensified side effects and potential toxicity.
Additionally, chronic alcohol consumption can contribute to fatty liver disease, impairing overall metabolic function and potentially negating Contrave’s weight loss benefits.
Gastrointestinal Issues
Alcohol is known to irritate the digestive system, and when combined with Contrave, it can exacerbate nausea, acid reflux, and the risk of ulcers.
Individuals who consume alcohol regularly may experience worsened gastrointestinal discomfort while taking Contrave, which can lead to long-term digestive complications if the combination continues over time.
Psychological and Behavioral Concerns
Impaired Judgment
Alcohol reduces inhibitions and impairs cognitive function, making it easier for individuals to engage in reckless behaviors.
For those taking Contrave to manage their weight, alcohol consumption can counteract the medication’s benefits by leading to overeating, engaging in risky situations, or neglecting weight loss plans altogether.
Mood Swings and Depression
Since bupropion is designed to regulate mood, alcohol’s depressive effects can interfere with this mechanism. Drinking alcohol while on Contrave can result in severe mood swings, exacerbating depression symptoms and potentially leading to suicidal thoughts.
Patients with a history of mood disorders should be especially cautious when considering alcohol consumption while taking Contrave.
Heightened Anxiety and Panic Attacks
The neurological effects of alcohol can increase feelings of anxiety, especially when combined with Contrave.
Individuals who are already prone to anxiety disorders may find that drinking alcohol intensifies their symptoms, leading to panic attacks or overwhelming stress that can disrupt daily life and overall well-being.
Binge-Eating Episodes
Contrave is designed to suppress appetite and reduce cravings, but alcohol consumption can disrupt this effect. Alcohol lowers self-control and increases hunger signals, leading individuals to engage in unplanned binge-eating episodes.
This can undermine weight loss progress and lead to frustration or feelings of failure in individuals using Contrave for weight management.
Medical Recommendations and Safer Alternatives
Healthcare Provider Consultation
Before starting Contrave, it is essential for individuals to discuss their alcohol consumption habits with their healthcare provider. This discussion will help determine the safest approach to using Contrave while minimizing potential risks associated with alcohol use.
Healthcare professionals may offer specific recommendations tailored to each patient’s medical history and weight loss goals.
Gradual Reduction of Alcohol Intake
For individuals who frequently consume alcohol, a gradual reduction before starting Contrave can help lower the risk of severe side effects.
Abruptly stopping alcohol intake, particularly for heavy drinkers, can cause withdrawal symptoms, which should be managed with medical supervision.
Safer Weight Loss Medications
Patients who drink alcohol regularly may need to consider alternative weight loss medications that do not carry the same level of risk as Contrave.
A healthcare provider can recommend weight loss drugs with fewer interactions, helping individuals achieve their health goals without compromising safety.
Behavioral Therapy and Counseling
Patients struggling with both weight loss and alcohol dependence may benefit from behavioral therapy or counseling.
These interventions can support long-term weight management strategies and address underlying emotional or psychological triggers contributing to excessive alcohol consumption or overeating.
The Role of Diet and Lifestyle in Contrave’s Effectiveness
Healthy Diet Choices
Maintaining a balanced diet is crucial for maximizing Contrave’s benefits. Avoiding high-fat foods can improve drug absorption and reduce gastrointestinal discomfort.
A diet rich in lean proteins, fiber, and vegetables can enhance weight loss results while supporting overall health.
Regular Exercise
Physical activity plays a vital role in weight management and overall well-being.
Combining Contrave with a consistent exercise regimen can improve cardiovascular health, enhance metabolism, and increase energy levels, leading to more effective weight loss results.
Proper Hydration
Staying hydrated is essential when taking Contrave, as dehydration can worsen side effects like nausea and dizziness.
Drinking adequate water supports metabolic function and prevents complications related to excessive alcohol or medication use.
Adequate Sleep
Sleep quality is a critical factor in weight loss and overall health.
Individuals taking Contrave should prioritize restful sleep, as sleep deprivation can lead to weight gain, increased cravings, and heightened stress levels that may counteract the medication’s benefits.
Frequently Asked Questions (FAQ) About Contrave and Alcohol Drug Interactions
Contrave is a weight loss medication that combines bupropion and naltrexone, both of which have specific effects on the brain and body. Because of its unique formulation, Contrave interacts with various substances, including alcohol, medications, and dietary choices.
Below are answers to some of the most commonly asked questions regarding Contrave, its interactions, and how to use it safely and effectively.
1. Can you take Contrave and drink alcohol?
It is strongly advised to avoid drinking alcohol while taking Contrave. Alcohol can intensify the side effects of Contrave, including dizziness, nausea, mood swings, and an increased risk of seizures. Additionally, since bupropion is associated with lowering the seizure threshold, combining it with alcohol—especially in large amounts or when suddenly stopping alcohol use—can significantly raise the risk of seizures.
Furthermore, alcohol can counteract the weight loss benefits of Contrave by lowering inhibitions and increasing the likelihood of overeating.
2. What medications should not be taken with Contrave?
Contrave interacts with several medications, and patients must consult their healthcare provider before combining it with other drugs. Opioid-based painkillers, such as oxycodone or morphine, should not be taken with Contrave due to naltrexone’s opioid-blocking effects, which can trigger severe withdrawal symptoms. Taking Contrave and Phentermine together can trigger drug interactions.
Additionally, antidepressants, certain beta blockers, antipsychotic medications, and diabetes treatments may require careful monitoring due to the risk of increased side effects or reduced effectiveness. Over-the-counter stimulants, energy supplements, and certain herbal remedies like St. John’s Wort may also interfere with Contrave’s effects. Even Contrave and melatonin can cause adverse drug interactions. In addition, Contrave and lisinopril drug interactions can occur, as alcohol affects blood pressure.
3. Is Contrave hard on the liver?
Both naltrexone and bupropion are metabolized in the liver, meaning that Contrave can put additional strain on liver function, particularly in individuals with pre-existing liver conditions. Patients with liver disease should consult their healthcare provider before starting Contrave to determine whether it is a safe option for them.
Chronic alcohol consumption can further increase the risk of liver damage, making it crucial to avoid excessive drinking while on Contrave. In most healthy individuals, liver function remains normal while taking the medication, but routine monitoring may be advised for those at higher risk.
4. Can I drink coffee while on Contrave?
Moderate coffee consumption is generally safe while taking Contrave; however, it is important to be mindful of caffeine intake. Contrave has stimulant-like effects due to bupropion, which can increase heart rate and blood pressure.
Consuming excessive caffeine from coffee, tea, or energy drinks may heighten these effects, leading to jitteriness, restlessness, or palpitations. If you experience increased anxiety, rapid heartbeat, or trouble sleeping while on Contrave, reducing caffeine intake may help alleviate these symptoms.
5. What to avoid while on Contrave?
While taking Contrave, it is essential to avoid alcohol due to the risk of seizures and intensified side effects. High-fat meals should also be minimized, as they can increase the absorption of Contrave, leading to a higher likelihood of nausea and dizziness. Opioid painkillers must be avoided, as naltrexone blocks opioid effects and can trigger withdrawal symptoms.
Other stimulants, such as energy drinks and weight loss supplements, should be used with caution, as they may increase heart rate and blood pressure. Patients should also consult their healthcare provider before taking new prescription or over-the-counter medications to prevent harmful drug interactions.
6. How to maximize weight loss on Contrave?
To maximize weight loss while taking Contrave, patients should adopt a comprehensive approach that includes a balanced diet, regular exercise, and lifestyle changes. Eating nutrient-dense foods that are low in processed sugars and unhealthy fats can improve the drug’s effectiveness. Consistent physical activity, such as cardio and strength training, enhances metabolism and supports sustainable weight loss. Staying hydrated and getting adequate sleep can also help the body regulate hunger and energy levels more effectively.
Additionally, following up with a healthcare provider or nutritionist can provide personalized recommendations to optimize results.
7. What is the downside of Contrave?
While Contrave can be effective for weight loss for compatible individuals, it is not without potential drawbacks. Some patients experience side effects such as nausea, dizziness, dry mouth, insomnia, or constipation, especially when first starting the medication.
Contrave also carries a risk of increasing blood pressure and heart rate, making it unsuitable for individuals with certain cardiovascular conditions. Additionally, because it contains bupropion, there is a potential for mood changes, anxiety, and, in rare cases, suicidal thoughts.
Patients should closely monitor their response to Contrave and consult their healthcare provider if they experience severe or persistent side effects.
Conclusion
The combination of Contrave and alcohol presents significant health risks that should not be underestimated. From increased susceptibility to seizures and cardiovascular complications to severe mental health impacts, the interaction between these substances can have profound consequences. Patients taking Contrave must be mindful of their alcohol intake, as even moderate consumption can disrupt the drug’s intended effects and heighten the risk of dangerous side effects.
Healthcare providers play a crucial role in guiding patients through safe weight loss treatments. Consulting a medical professional before consuming alcohol while on Contrave is essential in preventing severe adverse reactions. Individuals with pre-existing conditions such as high blood pressure, mood disorders, or liver issues should exercise particular caution.
For those committed to weight loss, prioritizing a balanced diet, regular exercise, and healthy lifestyle habits will yield far better results than relying on medication alone. Eliminating alcohol or significantly reducing consumption can support the effectiveness of Contrave, helping patients achieve their goals safely and sustainably.
Ultimately, informed decision-making and open discussions with healthcare professionals are key to ensuring a successful and safe weight loss journey.
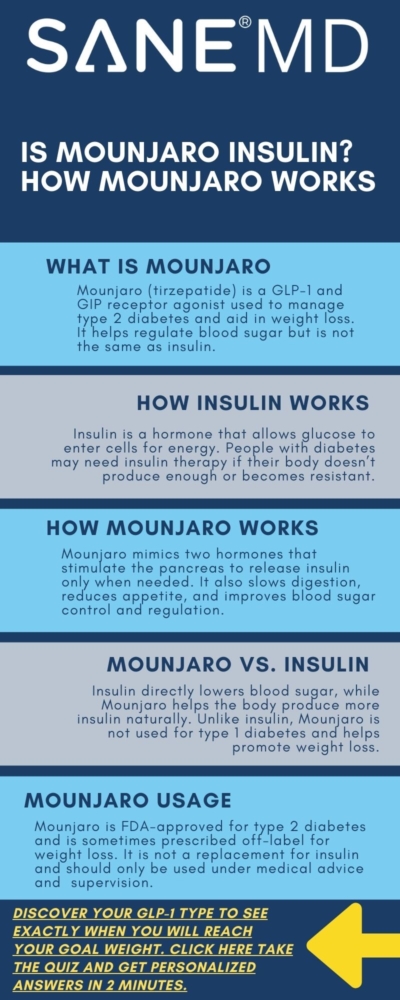
Is Mounjaro Insulin? How Mounjaro Aids Diabetes & Obesity
Mounjaro (tirzepatide) is a relatively new medication used for treating type 2 diabetes and aiding weight loss. Many people wonder, is Mounjaro insulin? The answer is no. Mounjaro is not insulin, but it is a GLP-1 medication that plays a key role in blood sugar control and weight management. Manufactured by Eli Lilly, this drug mimics two hormones that regulate insulin production and appetite.
This article explores how Mounjaro works, its effects on diabetes and obesity, and how it compares to other diabetes medications.
Key Takeaways
- Mounjaro is not insulin but helps regulate blood sugar levels and supports weight loss in individuals with type 2 diabetes.
- It mimics two hormones (GLP-1 and GIP) to enhance insulin production, slow digestion, and improve glycemic control.
- Mounjaro is an effective treatment for type 2 diabetes and obesity, potentially reducing the need for higher doses of insulin in some patients.
How Insulin Works
Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. It allows glucose from food to enter cells for energy.
When the body does not produce enough insulin or becomes resistant to it, blood sugar levels rise, leading to diabetes.
Role of Insulin in the Body
- Regulates blood sugar levels by helping glucose enter cells.
- Prevents excess sugar buildup in the bloodstream.
- Stores glucose in the liver for later use.
- Balances energy use by promoting or reducing glucose storage based on the body’s needs.
Individuals with type 1 diabetes require insulin injections because their bodies do not produce any insulin.
Those with type 2 diabetes may need insulin when their natural insulin production is insufficient for blood sugar regulation.
What Is Mounjaro?
What is Mounjaro used for? Mounjaro is a brand name for tirzepatide, a medication that helps regulate blood sugar levels and promote weight loss. It is an FDA-approved treatment for adults with type 2 diabetes, often prescribed alongside other diabetes medications or as an add-on therapy. See our article for more about Mounjaro eligibility.
Mounjaro is a GLP-1 (glucagon-like peptide-1) receptor agonist and also activates glucose-dependent insulinotropic polypeptide (GIP) receptors, making it unique compared to other diabetes drugs.
How Mounjaro Works for Type 2 Diabetes
Mounjaro is an innovative treatment for type 2 diabetes that works by mimicking the effects of two hormones, GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide).
These hormones play a crucial role in managing blood sugar levels by prompting the pancreas to increase insulin production when blood sugar levels are elevated. This process allows the body to better control blood sugar spikes, preventing extreme highs and lows that can contribute to diabetes complications.
Unlike insulin, which directly replaces the body’s natural insulin production, Mounjaro enhances insulin release only when needed, reducing the risk of low blood sugar episodes. Additionally, it slows digestion, meaning glucose from food is absorbed more gradually, keeping blood sugar levels steady.
Some patients on Mounjaro experience a reduced need for insulin dose adjustments, making it a helpful option for those seeking to avoid higher doses of injectable insulin.
Effects on Blood Sugar Control
- Increases insulin production only when blood sugar levels are elevated, reducing the risk of unnecessary insulin release.
- Lowers glucose production from the liver, which helps prevent excess blood sugar buildup.
- Slows digestion, ensuring a more gradual release of glucose into the bloodstream, preventing sharp blood sugar spikes.
- Enhances glycemic control, allowing patients with type 2 diabetes to maintain more stable blood sugar levels over time.
How Mounjaro Aids Weight Loss
Mounjaro has gained attention not only for its effectiveness in blood sugar control but also for its ability to promote significant weight loss for compatible individuals. By activating GLP-1 and GIP receptors, the medication affects both insulin regulation and appetite control. These hormones signal the brain to reduce hunger, leading to less food intake and making it easier for patients to maintain a caloric deficit.
Additionally, Mounjaro delays gastric emptying, meaning food stays in the stomach longer, keeping patients feeling full for extended periods. As a result, those taking Mounjaro tend to consume fewer calories, leading to more weight loss compared to traditional diabetes medications.
Clinical trials have demonstrated that patients using Mounjaro for type 2 diabetes experience substantial weight loss, with some losing up to 22.5% of their body weight.
Due to these findings, Eli Lilly developed Zepbound, a medication that contains the same active ingredient, tirzepatide, but is specifically FDA-approved for weight loss rather than type 2 diabetes. While Mounjaro is prescribed primarily for diabetes management, Zepbound is designed for certain individuals with obesity or those overweight with at least one weight-related condition. Both medications share similar mechanisms but are marketed for different treatment goals.
Mounjaro is often prescribed off-label for weight loss for certain individuals, even though Zepbound is now FDA-approved specifically for that purpose. Many healthcare providers still prescribe Mounjaro for weight loss because it has the same active ingredient (tirzepatide) as Zepbound and has already been widely used for type 2 diabetes patients who also experience significant weight loss.
Additionally, insurance coverage can play a role—some patients may find it easier to get Mounjaro covered under their plans, while Zepbound may have different restrictions.
Weight Loss Benefits
- Suppresses appetite, reducing overall food intake and caloric consumption.
- Delays stomach emptying, helping patients feel full for longer and minimizing overeating.
- Outperforms other diabetes medications in terms of more weight loss, making it a valuable choice for those managing both type 2 diabetes and obesity.
- Clinical trials report an average weight loss of up to 22.5%, significantly improving metabolic health and reducing the risk of diabetes-related complications.
Comparison: Mounjaro vs. Insulin
While insulin is essential for managing type 2 diabetes, Mounjaro offers an alternative approach for those who can still produce more insulin naturally. Unlike insulin glargine or insulin lispro, which directly supply insulin, Mounjaro helps the body use its own insulin more efficiently.
Key Differences
| Feature | Mounjaro | Insulin |
|---|---|---|
| Type | GLP-1 & GIP receptor agonist | Hormone replacement |
| Action | Enhances natural insulin production | Provides direct insulin dose |
| Administration | Weekly injections | Daily/multiple injections |
| For Type 1 Diabetes? | No | Yes |
| For Type 2 Diabetes? | Yes | Yes |
| Weight Effects | Promotes weight loss | May cause weight gain |
Dosage & Administration
Mounjaro is prescribed in a pen injector form, taken once a week in the upper arm, abdomen, or thigh. Patients may start on a lower dose and gradually increase to a maximum dose depending on the response.
Side Effects & Risks
Like any medication, people want to know if Mounjaro is safe and if it comes with potential side effects. The most commonly reported include:
- Diarrhea
- Nausea and vomiting
- Low blood sugar, especially when combined with basal insulin
- Hypoglycemia symptoms like dizziness, shakiness, or confusion
There are other potential side effects, possibly even hair loss. See our article, “Does Mounjaro cause hair loss?” to find out if this is a side effect of the medication or something else.
Who Should Take Mounjaro?
Mounjaro is prescribed for people with type 2 diabetes struggling with blood sugar control or those needing additional support for weight loss. However, it is not recommended for:
- People with Type 1 Diabetes
- Pregnant women
- Individuals with a history of pancreatitis
Frequently Asked Questions (FAQ)
Mounjaro (tirzepatide) is a relatively new medication for type 2 diabetes and obesity, often compared to insulin.
Below are some common questions about how it works, its effects on insulin resistance, and its benefits and drawbacks.
1. Is Mounjaro considered insulin?
No, Mounjaro is not insulin. It is a GLP-1 and GIP receptor agonist that helps regulate blood sugar levels by enhancing the body’s natural insulin production when needed. Unlike insulin, which directly lowers blood sugar by moving glucose into cells, Mounjaro stimulates insulin release, slows digestion, and reduces appetite.
It is often used in people with type 2 diabetes who still produce some insulin but need help managing their blood sugar control and weight loss.
2. What insulin is similar to Mounjaro?
Mounjaro does not have a direct insulin equivalent, but it is sometimes compared to insulin glargine (a long-acting insulin) or insulin lispro (a fast-acting insulin) because both are used for blood sugar control in type 2 diabetes.
However, Mounjaro works differently by stimulating the body to produce more insulin naturally, whereas insulin therapy supplies an external insulin dose. Other GLP-1 receptor agonists like Ozempic (semaglutide) and Trulicity (dulaglutide) share more similarities with Mounjaro than insulin does. For more information, check out our article, “Mounjaro vs Other Weight Loss Drugs.”
3. Does Mounjaro reverse insulin resistance?
Mounjaro can improve insulin sensitivity, but it does not completely reverse insulin resistance. By stimulating GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors, it helps the body use insulin more effectively. This can lead to better glycemic control, lower blood glucose, and reduced dependence on higher doses of insulin or other diabetes medications.
However, lifestyle changes such as diet and exercise remain crucial in managing insulin resistance long-term.
4. What does Mounjaro do to someone without diabetes?
For individuals without diabetes, Mounjaro primarily leads to weight loss by suppressing appetite, slowing digestion, and reducing food intake. It helps regulate blood sugar levels, but since non-diabetics typically do not have high blood sugar, its primary effect is appetite control. Some side effects, such as low blood sugar (hypoglycemia), nausea, and digestive discomfort, may still occur.
While Mounjaro is FDA-approved for type 2 diabetes, it is also being studied as a weight-loss treatment for obesity in non-diabetic individuals.
5. What does Mounjaro do for diabetics?
Mounjaro helps people with type 2 diabetes regulate their blood sugar levels by increasing insulin production when needed, slowing digestion, and reducing glucose production by the liver. This leads to improved glycemic control, fewer blood sugar spikes, and more weight loss. Many patients experience significant reductions in A1C levels and require lower doses of other diabetes medications or insulin.
Additionally, its once-weekly injection makes it a convenient option for certain patients. seeking an alternative to daily medications.
6. What are the cons of taking Mounjaro?
While Mounjaro offers significant benefits for blood sugar control and weight loss, it has some downsides. Common side effects include nausea, vomiting, diarrhea, and low blood sugar (especially when combined with insulin). Some patients may also experience injection site reactions or digestive discomfort as their body adjusts to the medication.
More serious risks include pancreatitis, gastrointestinal disorders, and potential thyroid tumors (observed in animal studies). It is not recommended for pregnant individuals or those with a history of pancreatic disease.
7. How long can you stay on Mounjaro for diabetes?
Mounjaro is designed for long-term use in people with type 2 diabetes, as long as it remains effective and well-tolerated. There is no strict time limit on treatment, but patients should have regular evaluations with their doctor to monitor blood sugar levels, weight, and potential side effects.
If blood sugar control improves significantly or weight stabilizes, a healthcare provider may adjust the dose or consider alternative treatments. Some patients stay on Mounjaro indefinitely if it continues to provide glycemic control and support weight loss.
Conclusion
Mounjaro is a breakthrough medication for type 2 diabetes and obesity, offering an alternative to insulin for blood sugar regulation. By acting on GLP-1 and glucose-dependent insulinotropic polypeptide, it supports glycemic control and significant weight loss. Patients considering taking Mounjaro should consult their pharmacist or healthcare provider to evaluate its benefits and risks.
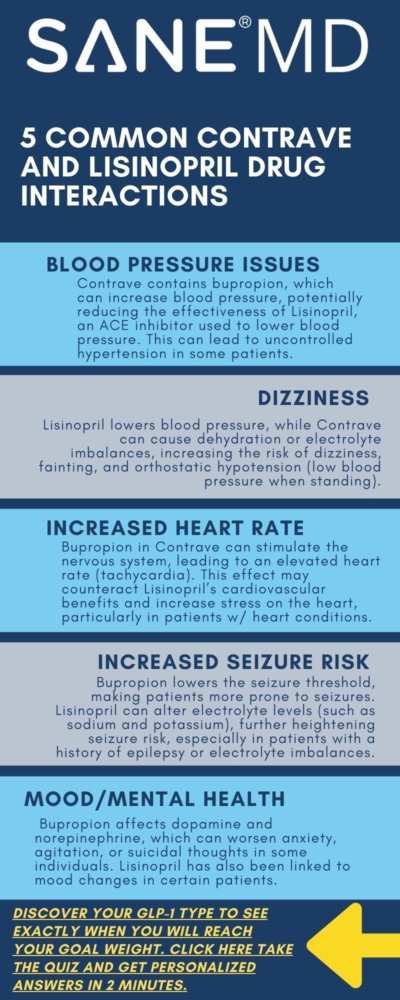
Contrave and Lisinopril Drug Interactions: Safe Combo?
Contrave and Lisinopril are two widely prescribed medications with different therapeutic uses. What does Contrave do? Contrave is commonly used for weight loss, while Lisinopril is a medication that helps treat high blood pressure and other cardiovascular conditions.
However, like many other drugs, there is a need to understand how these medications interact to ensure patient safety. Drug interactions can lead to unwanted side effects, reduced effectiveness, or increased risks associated with certain health conditions.
This article explores the potential Contrave and Lisinopril Drug Interactions, their effects on blood pressure, and what patients should know before taking them together.
Key Takeaways
- Contrave and Lisinopril may interact in ways that affect blood pressure regulation, requiring medical supervision.
- Patients should be aware of potential side effects, including nausea, vomiting, and dizziness, which may be heightened by combining these drugs.
- Consulting a doctor before starting Contrave while on Lisinopril is essential to minimize health risks and ensure safe use.
What Are Contrave and Lisinopril?
Contrave is a combination of bupropion and naltrexone that is prescribed to assist with weight loss by reducing appetite and affecting brain pathways involved in hunger and cravings. Naltrexone belongs to the drug class known as opioid antagonists, while bupropion is categorized as an antidepressant.
It is often recommended for certain individuals struggling with obesity or those with a high body mass index (BMI) who have related health conditions, such as high blood pressure or diabetes.
Lisinopril is an ACE inhibitor frequently prescribed for managing high blood pressure, treating heart failure, and enhancing survival rates following a heart attack. By relaxing blood vessels, it helps lower blood pressure and reduces the strain on the heart.
Potential Risks and Interactions Between Contrave and Lisinopril
| Interaction Category | Details |
|---|---|
| Blood Pressure Effects | Contrave (bupropion) can increase blood pressure, potentially counteracting Lisinopril’s effects. Monitoring is required. |
| Risk of Dizziness & Lightheadedness | Both drugs can cause dizziness, especially when standing quickly. Lisinopril lowers blood pressure, while Contrave may lead to dehydration. |
| Potential for Increased Heart Rate | Bupropion in Contrave may raise heart rate, counteracting Lisinopril’s cardiovascular benefits. Patients with heart conditions should be cautious. |
| Increased Risk of Seizures | Bupropion increases seizure risk, while Lisinopril can alter electrolyte levels, potentially worsening the risk. |
| Gastrointestinal Effects | Both drugs can cause nausea, vomiting, and digestive discomfort. Symptoms may be heightened when combined. |
| Mood & Mental Health Considerations | Bupropion can impact mood and increase suicidal thoughts. Lisinopril may also contribute to mood changes. |
| Alcohol Interaction | Alcohol can amplify side effects such as dizziness, drowsiness, and increased blood pressure. It also raises seizure risk with Contrave. |
| Other Drug Interactions | Contrave should not be combined with opioids, beta-blockers, or certain antidepressants. Lisinopril may interact with NSAIDs, lithium, and potassium supplements. |
How Do These Medications Interact?
Blood Pressure Considerations
Taking Contrave and Lisinopril together may result in fluctuations in blood pressure. Contrave, due to its bupropion component, can increase blood pressure, which may counteract the effects of Lisinopril. This can be particularly concerning for patients taking Lisinopril to treat high blood pressure.
Additionally, Lisinopril lowers blood pressure by dilating blood vessels, while bupropion can cause mild hypertensive effects. Patients with pre-existing high blood pressure should have their blood pressure closely monitored to ensure that the combination does not lead to dangerous fluctuations.
The renin-angiotensin system, which Lisinopril influences, plays a key role in blood pressure regulation by helping blood vessels contract or relax. On the other hand, bupropion, which affects dopamine and norepinephrine systems, can indirectly stimulate the sympathetic nervous system, potentially leading to increased heart rate and blood pressure.
This opposing mechanism makes it essential for patients taking both medications to have their blood pressure monitored regularly to prevent hypertensive crises or hypotensive episodes.
Risk of Dizziness and Lightheadedness
Patients combining these medications may experience dizziness or lightheadedness, particularly when standing up quickly. This is due to Lisinopril’s blood pressure-lowering effects, which may be exacerbated by Contrave’s potential to cause dehydration or electrolyte imbalances.
Dehydration can lead to a drop in blood pressure, which in turn increases the likelihood of dizziness and fainting. Patients are advised to stay well-hydrated and to avoid sudden movements when standing.
Furthermore, bupropion’s stimulant-like effects may contribute to dizziness, as it increases activity in the central nervous system, affecting balance and coordination. Patients who experience persistent dizziness should consult their doctor to adjust dosages or explore alternative medications that do not cause severe fluctuations in blood pressure.
Potential for Increased Heart Rate
Bupropion, a key ingredient in Contrave, can increase heart rate, potentially placing extra strain on the cardiovascular system when combined with Lisinopril. Since Lisinopril is meant to ease the burden on the heart by reducing blood pressure, the stimulating effects of bupropion on heart rate may counteract its benefits.
Patients with a history of heart conditions should consult their doctor before using these medications together to prevent cardiovascular complications.
Individuals with pre-existing tachycardia or arrhythmias should be particularly cautious, as bupropion can lead to palpitations and rapid heart rate. Medical attention should be sought immediately if a patient experiences an abnormally high heart rate or chest discomfort.
Deciding if Contrave is right for you demands careful consideration of these potential drug interactions.
Risks and Side Effects
Contrave drug interactions are many, including the following:
Increased Risk of Seizures
Bupropion has been linked to an increased risk of seizures, especially in patients with a history of seizure disorder. Since Lisinopril may alter electrolyte levels, particularly sodium and potassium, it could further predispose some patients to seizures.
Low sodium levels, also known as hyponatremia, can increase seizure risk, making it essential for patients to have their electrolyte levels monitored regularly.
Gastrointestinal Effects
Both medications may cause nausea, vomiting, and stomach discomfort. This combination could heighten the risk of severe stomach upset, especially when starting Contrave. Bupropion and naltrexone both act on the central nervous system, which can lead to nausea, while Lisinopril can cause digestive disturbances.
Patients experiencing persistent gastrointestinal side effects should consult their doctor to determine if dosage adjustments or alternative medications are necessary.
Mood and Mental Health Considerations
Patients with mental health conditions such as depression and anxiety should be cautious when taking Contrave and Lisinopril together. Bupropion, a component of Contrave, can interfere with mood regulation and may increase the risk of suicidal thoughts in some individuals.
Those with a history of depression should be closely monitored, particularly during the initial weeks of treatment. Lisinopril has also been reported to cause mood changes in some patients, further emphasizing the need for medical supervision.
Can You Drink Alcohol While Taking Contrave and Lisinopril?
Alcohol consumption while taking Contrave and Lisinopril is not recommended. Alcohol can interfere with the effectiveness of both drugs and increase the risk of side effects such as dizziness, drowsiness, and increased blood pressure.
Furthermore, alcohol use may increase the risk of seizures in patients taking Contrave. Since both medications affect blood pressure regulation, alcohol can compound these effects, leading to unpredictable fluctuations in blood pressure.
Patients are strongly advised to avoid alcohol or consume it in moderation only after discussing it with their healthcare provider.
Other Drugs That May Interact
Below are certain medicines that may also interact with Contrave:
Beta Blockers
Patients taking beta blockers alongside Lisinopril and Contrave should be cautious, as these medications affect heart rate and blood pressure regulation.
Beta blockers slow the heart rate, while Contrave can increase it, potentially leading to irregular heartbeat or cardiovascular stress.
Other Antidepressants
Taking Contrave with other antidepressants, including Wellbutrin SR, may increase the risk of side effects, including seizures and mood disturbances.
Certain antidepressants may also amplify the blood pressure-increasing effects of bupropion.
Opioid Medications
Since Contrave contains naltrexone, it blocks the effects of opioid-based medications, making them ineffective. This is especially relevant for individuals using opioids for pain management or opioid withdrawal treatment.
Patients currently on opioid therapy should not take Contrave without consulting their doctor, as this combination can lead to withdrawal symptoms.
Who Should Avoid This Drug Combination?
Patients with a history of liver problems, kidney disease, seizures, or heart conditions should consult a doctor before starting Contrave while on Lisinopril. The combination may also not be suitable for pregnant or breastfeeding individuals, as naltrexone and bupropion can pass into breast milk.
Individuals with uncontrolled high blood pressure or those at risk of cardiovascular events should be particularly cautious, as Contrave can elevate blood pressure.
Patients with a history of stroke, severe migraines, or metabolic disorders should also avoid combining these medications unless absolutely necessary.
Electrolyte imbalances caused by Lisinopril can heighten the risk of seizures, especially in patients predisposed to them due to bupropion’s effects.
A full assessment by a healthcare professional is essential before initiating this combination.
Alternative Weight Loss Options for Patients on Lisinopril
For patients who cannot take Contrave due to its interactions with Lisinopril, alternative weight loss treatments may be a safer option.
Several FDA-approved weight loss medications do not contain bupropion or naltrexone, making them more suitable for individuals with hypertension or heart-related conditions.
Other Prescription Medications
- Orlistat (Alli, Xenical): A lipase inhibitor that prevents fat absorption in the intestines, reducing overall caloric intake without affecting blood pressure or heart rate. Alli is an over-the-counter version of Orlistat.
- Liraglutide (Saxenda): A GLP-1 receptor agonist that promotes weight loss in certain individuals by regulating appetite and slowing digestion. It has been shown to lower blood pressure rather than increase it.
- Phentermine-Topiramate (Qsymia): A combination drug that suppresses appetite but must be used with caution in patients with hypertension.
Non-Prescription and Lifestyle Approaches
Patients on Lisinopril who wish to lose weight safely can benefit from lifestyle modifications, such as:
- Nutritional counseling: Reducing sodium intake can help control blood pressure while supporting weight loss.
- Regular physical activity: Moderate aerobic exercise, like brisk walking or swimming, can aid weight loss without putting excess strain on the cardiovascular system.
- Behavioral therapy: Working with a psychologist or dietitian to develop sustainable eating habits can improve long-term weight management.
Choosing a weight loss treatment tailored to individual medical needs ensures both safety and effectiveness.
Consulting a doctor before making changes to a medication regimen or diet plan is always recommended.
Monitoring and Safety Tips
- Regular blood pressure monitoring is crucial for patients taking both medications to detect any concerning changes early.
- Discuss any side effects with a doctor, particularly dizziness, nausea, or heart palpitations, to determine whether dosage adjustments are needed.
- Stop taking Contrave and seek medical advice if severe side effects such as irregular heartbeat, persistent vomiting, or suicidal thoughts occur.
Frequently Asked Questions (FAQ)
When taking prescription medications such as Contrave and Lisinopril, it’s important to understand how they interact with other drugs.
Many patients wonder whether they can safely combine these medications, as both can affect blood pressure and other bodily functions.
Below are answers to some of the most common questions regarding Contrave, Lisinopril, and potential drug interactions.
1. Can you take Contrave with blood pressure medicine?
Contrave can be taken with blood pressure medication, but it requires careful monitoring. Contrave contains bupropion, which can increase blood pressure in some patients, potentially counteracting the effects of antihypertensive medications like Lisinopril.
Doctors typically assess a patient’s baseline blood pressure before prescribing Contrave, especially if they are already taking medication to treat high blood pressure.
If the combination is deemed necessary, regular blood pressure monitoring is advised to ensure safe use. Patients with uncontrolled hypertension may need an alternative weight-loss treatment to minimize cardiovascular risks.
2. Can Lisinopril be taken with bupropion?
Lisinopril can generally be taken with bupropion, but caution is required due to the potential for blood pressure fluctuations and increased heart rate. Bupropion can lead to mild increases in blood pressure and heart rate, while Lisinopril works to lower blood pressure. In some individuals, this can create a balancing effect, but in others, it may cause unpredictable cardiovascular responses.
Additionally, Lisinopril can alter electrolyte levels, which may heighten the risk of seizures in patients taking bupropion, particularly those with a seizure disorder or a history of brain injuries. A doctor should evaluate the risks versus benefits before prescribing these medications together.
3. What medications should I avoid with Contrave?
Certain medications should be avoided while taking Contrave due to the risk of dangerous interactions. Opioid medications, such as oxycodone, hydrocodone, or morphine, should not be taken with Contrave, as its naltrexone component blocks opioid effects, potentially leading to sudden withdrawal symptoms.
Other antidepressants, particularly monoamine oxidase inhibitors (MAOIs) like phenelzine or tranylcypromine, should also be avoided due to the risk of hypertensive crisis and serotonin syndrome. Stimulants, such as amphetamine-based ADHD medications, may further increase heart rate and blood pressure, posing additional risks.
Patients should also be cautious with other drugs that affect mood or seizure threshold, including some antipsychotics and corticosteroids. Also, though not confirmed, Contrave and birth control drug interactions may occur, so you’ll need to be aware of this potential risk. Always consult a doctor before combining Contrave with other medications.
4. What medications should you avoid while taking Lisinopril?
Several medications should be avoided while taking Lisinopril to prevent potentially dangerous interactions. Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, can reduce Lisinopril’s effectiveness and may increase the risk of kidney damage.
Potassium supplements and potassium-sparing diuretics, such as spironolactone, should also be used cautiously, as Lisinopril can lead to high potassium levels, which may cause heart complications. Lithium, a medication used for mood disorders, can become toxic when taken with Lisinopril, as the drug affects lithium’s clearance from the body.
Additionally, other blood pressure medications, particularly angiotensin receptor blockers (ARBs) or direct renin inhibitors, may cause excessive blood pressure drops or kidney dysfunction when combined with Lisinopril. Patients should always inform their doctor about all the medications they are taking to avoid adverse effects.
Conclusion
Understanding Contrave and Lisinopril drug interactions is essential for patients considering taking these medications together. While they can be prescribed together under medical supervision, patients must be mindful of potential risks, including increased blood pressure, gastrointestinal side effects, and mood changes.
Consulting a doctor or pharmacist before starting Contrave is necessary to ensure safe and effective treatment, particularly for individuals managing high blood pressure, seizures, or other conditions. Always follow the prescribed dosage and be aware of potential interactions with other medications to minimize health risks.