Contrave and Tramadol Drug Interactions: Dangerous Duo?
Contrave and tramadol are two commonly prescribed medications, but their simultaneous use can pose significant health risks. Contrave is primarily used for chronic weight management for compatible individuals, while tramadol is an opioid analgesic used to relieve moderate to severe pain.
Both drugs affect neurotransmitter systems in the brain, leading to potential interactions that may increase the risk of seizures, high blood pressure, and serotonin syndrome. Understanding potential Contrave and tramadol drug interactions is crucial for patients taking both drugs.
Key Takeaways
- Increased Risk of Seizures: Taking Contrave and tramadol together may lower the seizure threshold, leading to an increased risk of seizures, particularly in individuals with a history of seizure disorder or other risk factors.
- High Blood Pressure Concerns: Both drugs can elevate blood pressure. Patients with preexisting high blood pressure or cardiovascular disease should call their healthcare provider before starting Contrave treatment.
- Potential for Serotonin Syndrome: The combination of Contrave and tramadol may increase serotonin levels, potentially leading to serotonin syndrome. Symptoms include confusion, rapid heart rate, and muscle rigidity, requiring immediate medical attention.
Understanding Contrave and Tramadol
Contrave: A Weight Loss Aid
Contrave is a combination of bupropion hydrochloride and naltrexone hydrochloride, two medications that influence brain chemistry to reduce food cravings. Bupropion doses are commonly used to treat depression and aid in smoking cessation, as it modulates dopamine and norepinephrine levels in the brain. However, this mechanism also affects the seizure threshold, increasing the risk of seizures, particularly in individuals predisposed to seizure disorders or those using high doses.
Naltrexone systemic exposure helps block opioid receptors in the brain, a mechanism originally used for opioid dependence and alcohol addiction. In the context of chronic weight management, naltrexone’s role is to reduce food cravings and binge-eating behaviors by modifying reward pathways. However, patients with severe hepatic impairment or a history of opioid use should exercise caution, as naltrexone can interfere with pain management and precipitate opioid withdrawal symptoms when combined with certain medications.
Despite its benefits in promoting weight loss, Contrave is not suitable for everyone. Individuals with high blood pressure, bipolar disorder, or a history of seizure disorder may face complications. Taking Contrave requires careful monitoring of patients to ensure safety, especially in those with preexisting conditions.
Tramadol: A Pain Reliever with Risks
Tramadol is an opioid pain reliever that has serotonin and norepinephrine reuptake inhibition properties, making it unique among opioids. This dual mechanism not only provides pain relief but also affects mood and energy levels. While tramadol is widely used for moderate to severe pain, it comes with notable risks, particularly its potential for opioid dependence and opioid withdrawal symptoms if suddenly discontinued.
Unlike stronger opioids, tramadol is often perceived as having a lower risk of addiction; however, it can still cause physical dependence over time. Patients using tramadol for an extended period may develop tolerance, requiring higher doses for the same pain-relieving effects. Additionally, the risk of serotonin syndrome occurs when tramadol is combined with other drugs that influence serotonin levels, such as Contrave.
Patients with a history of severe allergic reaction to opioids or those taking monoamine oxidase inhibitors should avoid tramadol, as the combination may result in life-threatening side effects. Furthermore, bupropion inhibits certain liver enzymes, potentially affecting how tramadol is metabolized in the body. This interaction can increase the drug’s potency, heightening the risk of side effects such as dizziness, nausea, and respiratory depression.
It is also crucial for individuals with severe renal impairment or moderate hepatic impairment to consult their healthcare provider before using tramadol, as compromised kidney or liver function may lead to increased risk of toxicity. Patients should never suddenly stop drinking alcohol while on tramadol, as alcohol can intensify central nervous system depression and increase the risk of seizures.
Both Contrave treatment and tramadol have their place in medical therapy, but when used together, the combination requires careful oversight to avoid dangerous interactions.
Contrave and Tramadol Drug Interactions
| Interaction | Description |
|---|---|
| Increased Risk of Seizures | Both medications lower the seizure threshold, increasing the likelihood of seizures, especially in individuals with a history of epilepsy or other risk factors. |
| High Blood Pressure Concerns | Both Contrave and tramadol can elevate blood pressure, increasing the risk of hypertensive crises, particularly in individuals with preexisting cardiovascular conditions. |
| Potential for Serotonin Syndrome | The combination may lead to serotonin syndrome, a potentially life-threatening condition characterized by confusion, rapid heartbeat, muscle rigidity, and excessive sweating. |
| Impact on Mental Health | Bupropion (in Contrave) can worsen major depressive disorder or bipolar disorder, while tramadol is linked to neuropsychiatric adverse events, including mood swings and suicidal ideation. |
| Drug Metabolism and Systemic Exposure | Bupropion affects tramadol’s metabolism, increasing systemic exposure and leading to heightened side effects such as dizziness, nausea, and respiratory depression. |
| Allergic Reactions and OTC Interactions | Both drugs can cause allergic reactions ranging from mild rashes to severe anaphylaxis. Over-the-counter medications like NSAIDs and decongestants may interact negatively with these drugs. |
The Risks of Taking Contrave and Tramadol Together
Increased Risk of Seizures
Both bupropion naltrexone and tramadol lower the seizure threshold, making seizures more likely, especially in individuals with seizure disorder or certain risk factors such as traumatic brain injury or excessive alcohol use.
Tramadol’s dopamine agonist effects further complicate the situation. Patients taking bupropion already face a heightened risk of seizures, which is amplified when tramadol is introduced. The boxed warning alerts doctors to the increased seizure risk associated with bupropion therapy, emphasizing the need for careful monitoring.
Blood Pressure Concerns
High blood pressure is a well-documented side effect of Contrave, as bupropion hydrochloride increases systemic exposure to norepinephrine, leading to severely high blood pressure in some cases. When combined with tramadol, which also affects blood pressure regulation, there is an even greater increased risk of hypertensive crises.
Starting Contrave treatment requires monitoring blood pressure levels regularly, particularly in patients with a history of cardiovascular disease or severe renal impairment. Patients should call their healthcare provider if they experience persistent headaches, dizziness, or chest pain while on Contrave tablets.
Serotonin Syndrome Risk
Serotonin syndrome occurs when excessive serotonin accumulates in the brain, leading to serious health issues. Since both tramadol and Contrave influence serotonin levels, the combination may trigger serotonin syndrome. Symptoms include agitation, sweating, tremors, rapid heartbeat, and loss of coordination.
Patients taking Contrave and tramadol should be aware of this rare but potentially life-threatening condition. Call your healthcare provider right away if symptoms develop.
Additional Drug Interaction Concerns
Impact on Mental Health
Bupropion, found in Contrave, is commonly used to treat depression and has been linked to major depressive disorder and bipolar disorder exacerbations. Tramadol, on the other hand, is associated with serious neuropsychiatric adverse events, including mood changes and suicidal ideation.
For young adults, the combination can be particularly risky, as bupropion inhibits the reuptake of dopamine and norepinephrine, potentially worsening mental health conditions. Patients should call their healthcare provider before using these medications together.
Drug Metabolism and Systemic Exposure
The combination of Contrave and tramadol can affect systemic exposure to both drugs, altering their effectiveness and safety. Bupropion exposure increases when taken with tramadol, potentially leading to heightened side effects such as insomnia, agitation, and nausea.
Additionally, Contrave treatment can interfere with opioid withdrawal symptoms, making tramadol less effective for pain relief. This issue is especially problematic for patients recovering from opioid dependence or undergoing smoking cessation treatment.
Allergic Reactions and Over-the-Counter Drug Interactions
Both medications can cause allergic reactions, ranging from mild skin rashes to severe anaphylaxis. Patients experiencing swelling, difficulty breathing, or hives should seek immediate medical attention.
Over-the-counter drugs such as NSAIDs, decongestants, and certain cold medications may interact with Contrave and tramadol. Monitor patients carefully when introducing new medications.
Patient Safety and Precautions
Monitoring for Side Effects
Patients taking Contrave or tramadol should be aware of potential side effects and report any unusual symptoms to their healthcare provider right away.
Common side effects of Contrave include nausea, headache, dizziness, and increased heart rate. Tramadol can cause drowsiness, constipation, and dizziness. If severe adverse effects such as difficulty breathing, severe allergic reactions, or irregular heartbeat occur, immediate medical attention is necessary.
When to Stop Taking Contrave or Tramadol
It is important not to discontinue Contrave or tramadol abruptly without consulting a healthcare provider. Stopping Contrave suddenly may lead to withdrawal symptoms such as irritability, mood swings, and changes in appetite.
Similarly, discontinuing tramadol abruptly can cause severe opioid withdrawal symptoms, including nausea, sweating, anxiety, and muscle pain. Patients should work with their healthcare provider to taper their dosage if discontinuation is necessary.
Handling Missed Doses
If a dose of Contrave or tramadol is missed, patients should take it as soon as they remember. However, if it is close to the time for the next dose, the missed dose should be skipped to avoid double dosing.
Taking more than the prescribed dose can increase the risk of seizures, high blood pressure, and other adverse effects. If multiple doses are missed, consult a healthcare provider for guidance.
Special Populations and Contraindications
Contrave Interactions with Multiple Drugs
There are more than 200 known drugs that interact with Contrave. For example, in taking Contrave and phentermine together, drug interactions can occur and become quite serious. Taking Contrave and Topamax together can also lead to drug interactions, as can taking Contrave and Ozempic together; however, few studies have ever investigated the possible interactions between these two drugs. There are also Contrave and Lisinopril Drug Interactions you should be aware of.
Pregnant and Breastfeeding Women
Both drugs can pass into breast milk, potentially harming a nursing infant. Women who are pregnant or breastfeeding should consult their healthcare provider before using either medication.
Patients with Hepatic or Renal Impairment
Patients with severe hepatic impairment or moderate hepatic impairment should avoid taking Contrave and tramadol together, as both medications rely on liver metabolism.
Similarly, individuals with severe renal impairment should be cautious, as impaired kidney function can lead to drug accumulation and increased toxicity.
Alcohol Use and Withdrawal Risks
Patients who suddenly stop drinking alcohol or have suddenly stopped drinking alcohol in the past may face an increased risk of seizures when using Contrave or tramadol. Alcohol withdrawal itself lowers the seizure threshold, compounding the dangers associated with these medications.
Patients taking Contrave should avoid alcohol consumption, as high-fat meals and alcohol can increase the risk of adverse reactions.
Safer Alternatives and Precautions
When considering the use of Contrave and tramadol together, understanding safer alternatives and precautionary measures is essential to minimize risks and enhance treatment efficacy.
Certain individuals, particularly those with underlying health conditions, may require modifications to their treatment plans to avoid severe side effects.
Medication Adjustments
A dosage adjustment may be necessary for individuals at higher risk of side effects, including those with bipolar disorder, high blood pressure, severe hepatic impairment, or a history of seizures. Patients with moderate hepatic impairment or severe renal impairment should also be monitored closely, as both Contrave and tramadol are metabolized by the liver and excreted through the kidneys.
Reduced clearance of these medications may lead to increased systemic exposure, elevating the risk of adverse reactions such as nausea, dizziness, and excessive sedation.
Additionally, individuals who have suddenly stopped drinking alcohol or have a history of alcohol dependence should proceed with caution, as abrupt alcohol cessation can increase the risk of seizures when combined with bupropion hydrochloride found in Contrave. Adjustments to Contrave treatment may be necessary to ensure that the seizure threshold is not further lowered.
Patients should never alter their dosage without consulting their healthcare provider, as incorrect dosing can lead to severely high blood pressure, opioid withdrawal symptoms, or worsening of underlying conditions. If a patient experiences adverse reactions such as tremors, confusion, irregular heartbeat, or difficulty breathing, they should seek medical attention immediately.
Monitoring and Medical Guidance
Physicians should monitor patients closely when prescribing Contrave and tramadol together, particularly in individuals at risk of serotonin syndrome, seizure disorder, or opioid dependence. Routine check-ups and blood pressure monitoring are essential, as Contrave treatment is known to increase the risk of high blood pressure, which may be compounded by tramadol’s effects on the central nervous system.
Patients with a history of major depressive disorder or bipolar disorder should be monitored for serious neuropsychiatric adverse events, including mood swings, hallucinations, or suicidal ideation. Since bupropion inhibits the reuptake of dopamine and norepinephrine, it may interact with tramadol’s effects on serotonin levels, potentially causing serotonin syndrome. Symptoms such as excessive sweating, agitation, rapid heartbeat, or muscle rigidity should be reported to a healthcare provider right away.
A medication guide should be provided to ensure that patients understand potential risks, necessary precautions, and warning signs of serious side effects. This guide should include instructions on how to properly take the medication, what substances to avoid (such as over-the-counter drugs that increase blood pressure), and when to contact a healthcare provider.
If adverse effects occur, patients should call their healthcare provider right away to discuss safer alternatives. In some cases, an alternative pain management strategy may be needed, such as switching from tramadol to a non-opioid pain reliever like acetaminophen or ibuprofen. Similarly, for individuals experiencing intolerable side effects from Contrave, adjustments to their reduced calorie diet or a change in weight management medication may be recommended.
By taking these precautionary steps, patients can reduce the likelihood of experiencing serious adverse reactions and optimize the safety and effectiveness of their treatment regimen.
Frequently Asked Questions (FAQ)
When considering the use of Contrave and tramadol together, it is essential to understand their potential interactions and risks. These medications affect brain chemistry in different ways, and their combined use can lead to severe side effects, including an increased risk of seizures, high blood pressure, and opioid withdrawal symptoms.
Below are some of the most frequently asked questions regarding Contrave, tramadol, and their interactions.
1. Can you take tramadol and Contrave together?
Taking tramadol and Contrave together is generally not recommended due to the increased risk of seizures and serotonin syndrome. Both medications can lower the seizure threshold, making seizures more likely, particularly in individuals with a history of epilepsy or other neurological conditions.
Additionally, tramadol affects serotonin levels, and when combined with Contrave, the risk of serotonin syndrome occurs, which can lead to confusion, rapid heartbeat, and muscle rigidity. Always consult your healthcare provider before combining these medications.
2. What pain medicine can I take with Contrave?
If you need pain relief while taking Contrave, safer alternatives to tramadol should be considered. Non-opioid pain relievers such as acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen may be better choices.
However, it is still important to call your healthcare provider before using any new medication to ensure it does not interact with Contrave or contribute to side effects such as high blood pressure or increased risk of seizures.
3. Can I take bupropion and tramadol together?
Taking bupropion and tramadol together is generally discouraged due to the potential for dangerous interactions. Bupropion inhibits the metabolism of certain drugs, which can cause increased levels of tramadol in the body, heightening the risk of serotonin syndrome and severe allergic reaction.
Additionally, both medications lower the seizure threshold, significantly increasing the risk of seizures. If pain management is needed, alternative pain medications should be discussed with a healthcare provider.
4. What medications should I avoid with Contrave?
Several medications should be avoided while taking Contrave due to potential interactions. Opioid-containing medicines, such as oxycodone or hydrocodone, should not be used because naltrexone systemic exposure blocks opioid receptors, leading to withdrawal symptoms. Additionally, monoamine oxidase inhibitors (MAOIs), certain antidepressants, and drugs that affect dopamine levels should be used with caution.
Always inform your healthcare provider about all over-the-counter drugs, supplements, and prescriptions you are taking before starting Contrave treatment.
5. What happens if you take opioids with Contrave?
Taking opioids while on Contrave can lead to opioid withdrawal symptoms, as naltrexone hydrochloride blocks opioid receptors, preventing the effects of opioid medications. This can result in severe withdrawal reactions, including nausea, vomiting, sweating, anxiety, and muscle pain.
If you are taking opioids for pain management, discuss alternatives with your healthcare provider right away before starting Contrave.
6. What medications should not be taken with Contrave?
In addition to opioids, Contrave should not be taken with drugs that increase the risk of seizures, such as certain antidepressants, antipsychotics, or stimulants. Monoamine oxidase inhibitors (MAOIs) should be avoided, as their combination with Contrave may lead to dangerously high blood pressure.
Patients with severe hepatic impairment or bipolar disorder should consult their healthcare provider before using Contrave, as it may worsen these conditions.
When in doubt, always call your healthcare provider before starting any new medication while on Contrave to ensure your safety and avoid potential adverse reactions.
Conclusion
The combination of Contrave and tramadol poses significant risks, including increased risk of seizures, high blood pressure, and serotonin syndrome. Taking Contrave with tramadol requires careful monitoring and medical supervision.
Patients should discuss their medical history, including bipolar disorder, seizure disorder, and any past allergic reactions, with their healthcare provider before using these medications together.
Ultimately, understanding the potential dangers of contrave and tramadol drug interactions is crucial for making informed decisions about treatment. If you are considering using both medications, consult your healthcare provider right away to evaluate safer options for managing pain and weight loss effectively.
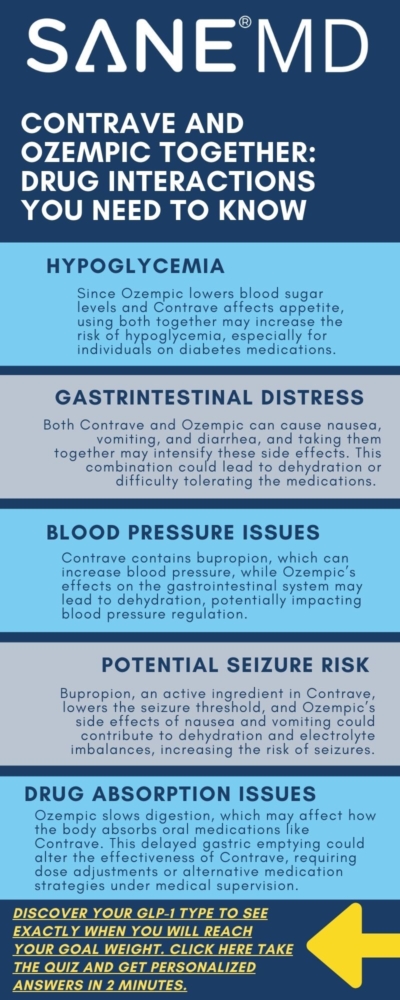
Contrave and Ozempic Together: Drug Interactions Explained
The combination of Contrave and Ozempic for weight loss has gained attention among individuals seeking effective chronic weight management solutions. Both medications are FDA-approved and offer different mechanisms for addressing excess body weight. Contrave suppresses appetite by targeting the brain’s reward system, reducing cravings and emotional eating. Ozempic, a GLP-1 receptor agonist, influences gut hormones to slow digestion, regulate blood sugar levels, and promote weight loss.
However, if taking Contrave and Ozempic together, drug interactions may occur, which raises questions about drug interactions, safety, and effectiveness. The potential benefits of combining these two weight loss medications must be weighed against one’s weight loss drug type (quiz here) and the risks of side effects, such as low blood sugar levels, gastrointestinal discomfort, and blood pressure fluctuations.
Individuals considering this combination should consult a healthcare provider to determine whether it aligns with their individual health needs.
Key Takeaways
- Contrave and Ozempic work differently—Contrave affects appetite control, while Ozempic helps regulate blood sugar levels and reduce food intake.
- Drug interactions may occur, leading to increased risks of low blood sugar, high blood pressure, and gastrointestinal issues.
- A healthcare provider should be consulted before combining these medications to assess potential risks, especially for individuals with a personal or family history of medical conditions.
How Contrave and Ozempic Work for Weight Loss
Understanding Contrave
Contrave is a combination medication consisting of bupropion and naltrexone. Bupropion is an antidepressant that influences appetite control, while naltrexone helps regulate food intake and cravings. Together, these components impact the brain’s reward system, reducing the urge to eat in response to stress or emotional triggers.
Contrave is commonly prescribed for individuals who struggle with weight loss maintenance due to emotional eating or difficulty controlling hunger. If you’re wondering how long Contrave stays in your system, check out our guide for detailed insights into its duration and metabolism.
How Ozempic Works
Ozempic is a GLP-1 receptor agonist that mimics gut hormones to help regulate blood sugar levels and support long-term weight management. It slows digestion, making compatible individuals feel full for longer periods, which contributes to weight reduction.
Additionally, Ozempic plays a significant role in managing blood sugar levels, making it a preferred option for individuals with diabetes medications. Unlike Contrave, which is an oral medication, Ozempic is administered through weekly injections.
Comparing Ozempic vs Contrave
The Ozempic vs Contrave debate often centers on how these weight loss drugs compare in terms of effectiveness and mechanism. While Contrave suppresses appetite by altering neurotransmitter activity, Ozempic reduces food cravings and regulates digestion.
Both medications have been shown to support significant weight loss, but their effectiveness varies based on an individual’s initial body weight, personal or family history, and other diabetes medications.
Contrave vs. Ozempic Comparison Table
| Feature | Contrave | Ozempic |
|---|---|---|
| Medication Type | Combination of bupropion and naltrexone | GLP-1 receptor agonist |
| Mechanism of Action | Affects brain’s reward system to reduce appetite and cravings | Mimics gut hormones to regulate blood sugar and slow digestion |
| How It Works | Suppresses appetite by altering neurotransmitter activity | Reduces hunger and prolongs fullness |
| Administration | Oral tablet taken daily | Weekly injection |
| Primary Benefits | Reduces emotional eating and food cravings | Weight loss through appetite suppression and blood sugar regulation |
| Potential Side Effects | Nausea, dizziness, insomnia, high blood pressure, mood changes | Nausea, vomiting, diarrhea, risk of low blood sugar, potential thyroid tumors |
| Ideal Candidates | Individuals struggling with emotional eating or compulsive cravings | Individuals with insulin resistance or type 2 diabetes |
| Warnings | Not recommended for those with seizure disorders, uncontrolled high blood pressure, or opioid use | Caution for those with a personal or family history of thyroid cancer or gastrointestinal disorders |
Psychological and Behavioral Considerations in Weight Loss
Achieving and maintaining long-term weight management is not just about calorie reduction and exercise—it is deeply influenced by psychological and behavioral factors. Many individuals struggle with appetite control, emotional eating, and impulse-driven food cravings, which can make sustained weight loss challenging.
Medications like Contrave target these psychological components, offering a neurochemical approach to weight loss that goes beyond simple dietary adjustments.
How Contrave Influences Emotional Eating and Behavior
Contrave is unique among weight loss medications because it directly impacts the brain’s reward system, particularly in individuals who eat in response to stress, emotions, or environmental cues. The medication combines bupropion and naltrexone, both of which influence dopamine pathways that regulate mood, motivation, and food cravings. Bupropion, an antidepressant, is known to reduce compulsive behaviors, while naltrexone, typically used for addiction treatment, helps diminish food-related pleasure responses.
Together, they work to break the cycle of emotional eating by dampening the brain’s desire for comfort foods and excessive calorie consumption.
By modifying how the brain perceives food rewards, Contrave helps individuals develop healthier eating patterns, allowing them to recognize real hunger cues rather than responding to emotional or habitual eating triggers.
This can be especially beneficial for those who have spent years struggling with unconscious eating habits or binge-eating behaviors.
The Role of Habit Formation in Weight Loss Success
Behavioral psychology suggests that habit formation is a critical factor in weight loss maintenance. Most people attempting to lose weight have deeply ingrained eating patterns and lifestyle habits that contribute to their difficulties in sustained weight reduction.
For instance, someone who eats in response to stress, boredom, or social situations may have conditioned themselves to associate food with emotional relief.
Contrave assists in disrupting these conditioned behaviors, making it easier for certain individuals to adopt healthier coping mechanisms. However, medication alone cannot replace the need for behavioral adjustments. Successful long-term weight loss requires conscious effort to replace unhealthy habits with sustainable alternatives, such as:
- Mindful eating – Becoming aware of hunger and fullness signals instead of eating out of habit.
- Stress management – Using exercise, meditation, or other relaxation techniques instead of turning to food.
- Structured meal planning – Preparing balanced meals in advance to avoid impulsive food choices.
Developing these new habits while taking Contrave can reinforce appetite control and food regulation, leading to a more sustainable weight loss journey.
Emotional Triggers and Their Impact on Weight Loss
For many individuals, emotional eating is a primary obstacle to achieving successful weight loss. Common triggers include stress, sadness, loneliness, or even celebrations, which can lead to episodes of overeating or binge eating. Contrave reduces cravings and food-related pleasure responses, making it easier to resist emotional eating urges.
However, medication cannot fully eliminate emotional triggers—it can only reduce their intensity. A comprehensive weight loss strategy should include behavioral therapy, cognitive restructuring, and self-awareness exercises to help individuals:
- Identify their primary emotional eating triggers.
- Develop alternative coping mechanisms for dealing with emotions without food.
- Strengthen self-regulation through consistent monitoring and reflection.
Those who use Contrave in combination with counseling or cognitive behavioral therapy (CBT) often see greater weight loss maintenance because they address both the biological and psychological aspects of eating behavior.
Long-Term Adherence and Weight Loss Maintenance
One of the biggest challenges in weight reduction is maintaining results after initial body weight loss. Studies show that many individuals regain lost weight within a few years due to a return to old habits and metabolic adaptations.
The key to weight loss maintenance is long-term adherence to healthy lifestyle changes, supported by behavioral consistency and medical interventions when necessary.
Contrave may help sustain weight loss maintenance by preventing the return of compulsive eating patterns, but individuals must also:
- Continue practicing appetite control strategies learned during weight loss.
- Maintain a healthy diet and regular physical activity.
- Seek ongoing support from a healthcare provider, dietitian, or therapist to navigate weight-related challenges.
By addressing both the neurological and behavioral components of weight management, individuals can achieve lasting changes in their relationship with food. When combined with structured habit formation, emotional regulation strategies, and long-term adherence plans, Contrave and other weight loss medications can become valuable tools for sustainable weight reduction and overall well-being.
Can You Take Contrave and Ozempic Together?
The possibility of taking Contrave and Ozempic together has intrigued individuals looking for additional benefits in their weight loss journey. Given their different mechanisms, some believe the combination could enhance average weight loss results.
Unlike taking Contrave and Topamax together, the combination of Contrave and Ozempic is not widely studied in clinical trials, meaning its long-term effects remain uncertain.
How Drug Interactions May Affect Metabolism and Blood Sugar
Using Contrave and Ozempic together may result in interactions that alter metabolism, hunger regulation, and insulin sensitivity. While Ozempic primarily influences gut hormones to regulate blood sugar levels, Contrave impacts neurotransmitters that contribute to appetite control. The combination could lead to unintended metabolic effects, such as increased insulin sensitivity, resulting in low blood sugar levels.
Moreover, individuals taking blood pressure medications, antidepressants, or other diabetes medications should be cautious, as Contrave’s bupropion component interacts with certain drugs used for depression, anxiety, and cardiovascular disease. The combination may increase the risk of high blood pressure, irregular heartbeat, or mood-related side effects, making it critical to consult a healthcare provider before initiating both medications.
Potential Risks and Side Effects
Like taking Contrave and Phentermine together, drug interactions between Contrave and Ozempic introduce the possibility of intensified side effects. Some individuals may experience abdominal pain, nausea, vomiting, or diarrhea, especially when first starting the medications. Additionally, both drugs can influence blood pressure, meaning those with high blood pressure should be particularly cautious.
A major concern with Ozempic is its association with thyroid tumors, including medullary thyroid carcinoma. Studies have suggested a possible link between GLP-1 receptor agonists and thyroid c cell tumors, making it crucial for individuals with a family history of thyroid cancer to avoid this medication. Similarly, Contrave contains bupropion, which lowers the seizure threshold, making it unsuitable for individuals with seizure disorders.
Another important risk is low blood sugar, particularly for individuals with diabetes management concerns. Ozempic is known to impact blood sugar levels, and when combined with Contrave, it may lead to low blood sugar levels, causing dizziness, confusion, and even loss of consciousness. Individuals experiencing difficulty breathing or allergic reactions should seek medical attention immediately.
Alternative Treatment Approaches for Weight Loss
For individuals who are not suitable candidates for Contrave and Ozempic together, alternative treatment options exist.
Lifestyle modifications remain the foundation of long-term weight management. A reduced calorie diet, regular physical activity, and behavioral therapy can significantly improve weight loss maintenance and metabolic health.
Additionally, other FDA-approved weight loss drugs such as Saxenda (liraglutide), Wegovy (semaglutide), and Qsymia (phentermine-topiramate) provide effective alternatives. These medications work through different mechanisms, including appetite suppression and gut hormone regulation, and may be safer options for individuals with certain medical conditions.
For individuals with severe obesity or weight-related comorbidities, bariatric surgery might be a viable solution. Procedures such as gastric bypass or sleeve gastrectomy offer significant weight loss and improve conditions like high blood pressure and diabetes management. Consulting a healthcare provider is essential for determining the best approach for weight reduction based on individual health considerations.
Frequently Asked Questions (FAQ)
Combining Contrave and Ozempic for weight loss raises many questions regarding safety, effectiveness, and potential drug interactions. Both medications work through different mechanisms, and their combined use should always be guided by a healthcare provider.
Below are some of the most common questions regarding these medications, including their compatibility, interactions, and comparative effectiveness for weight loss.
1. Can I take Contrave and Ozempic at the same time?
Yes, but only under the supervision of a healthcare provider. While Contrave and Ozempic work differently—Contrave targets appetite control, while Ozempic regulates blood sugar levels—combining them may increase the risk of side effects such as low blood sugar, nausea, and gastrointestinal discomfort. There are limited clinical trials examining the long-term effects of taking these two drugs together, so careful monitoring is essential.
Individuals with a personal or family history of thyroid cancer, seizure disorders, or cardiovascular disease should be particularly cautious. It is crucial to discuss the potential benefits and risks with your doctor before starting this combination.
Can I take bupropion and Ozempic together?
Bupropion, an active ingredient in Contrave, is sometimes prescribed separately for depression and smoking cessation, and it may be taken alongside Ozempic in certain cases. However, both medications can impact metabolism, appetite, and neurotransmitter activity, which may lead to unexpected drug interactions. One concern is that bupropion lowers the seizure threshold, which, when combined with Ozempic’s potential for nausea and vomiting, could increase the risk of seizures in susceptible individuals.
Additionally, the effects of blood sugar regulation may be altered, requiring close monitoring. Always consult a medical provider before using these medications together to ensure safety and effectiveness.
2. What medications should not be taken with Contrave?
Contrave interacts with several medications, making it important to review your medical history before starting this treatment. Bupropion, one of the active ingredients, can interact with antidepressants, seizure medications, and drugs that affect dopamine or serotonin levels, increasing the risk of mood disturbances, high blood pressure, or seizures. Opioid medications should also be avoided, as Contrave contains naltrexone, which can block the effects of opioids and cause withdrawal symptoms in individuals taking painkillers. Additionally, Contrave can impact blood pressure and may not be suitable for those on hypertension medications.
Always provide your healthcare provider with a complete list of current medications before starting Contrave.
3. What medications should be avoided while on Ozempic?
Ozempic may interact with medications that affect blood sugar levels, including insulin, sulfonylureas (like glipizide), and other diabetes medications. Combining these can increase the risk of low blood sugar levels (hypoglycemia), which may cause dizziness, confusion, or fainting. Additionally, drugs that slow gastric emptying, such as certain oral contraceptives or opioid pain relievers, may be affected by Ozempic, as it delays digestion. Patients taking thyroid medications or those with a personal or family history of thyroid cancer should also exercise caution, as GLP-1 receptor agonists have been linked to thyroid tumors in animal studies.
A medical provider can help determine whether any of your current prescriptions pose a risk when combined with Ozempic.
4. Can you take bupropion and Ozempic together?
Yes, but with caution and medical supervision. Since bupropion is a component of Contrave, this question is similar to whether Contrave and Ozempic can be taken together. Bupropion influences appetite, mood, and metabolism, while Ozempic regulates gut hormones to control blood sugar levels. Their combination could lead to nausea, dizziness, or fluctuations in blood pressure. Individuals with a history of seizures, eating disorders, or major depressive episodes should be especially cautious when taking bupropion with Ozempic, as it can exacerbate neurological side effects.
Consultation with a healthcare provider is crucial to determine whether this combination is safe for your specific health profile.
5. Is Contrave better than Ozempic for weight loss?
Neither medication is inherently better for weight loss; rather, their effectiveness depends on an individual’s body weight, metabolic needs, and medical history. Contrave primarily helps with appetite suppression and emotional eating, making it ideal for those who struggle with food cravings and impulse control.
Ozempic, on the other hand, mimics gut hormones to slow digestion and regulate blood sugar levels, which may be more effective for individuals with insulin resistance or type 2 diabetes. Studies show that Ozempic can lead to an average weight loss of 10-15% of initial body weight, while Contrave users typically lose 5-10% of their initial body weight.
If a patient has high blood pressure, seizure disorders, or difficulty with impulse eating, one drug may be preferable over the other. The best approach is to discuss these options with a healthcare provider to determine which medication aligns with your long-term weight management goals.
Final Thoughts: Should You Take Contrave and Ozempic Together?
The decision to take Contrave and Ozempic together should be made carefully, considering the potential benefits and risks. While some individuals may experience greater weight reduction, the possibility of drug interactions, thyroid tumors, and cardiovascular events cannot be ignored.
Individuals with a personal or family history of thyroid cancer, seizure disorders, or heart disease should be particularly cautious before considering this combination. Consulting a healthcare provider immediately is essential to assess suitability based on individual health needs, personal or family history, and overall weight management goals.
Ultimately, successful weight loss is best achieved through a combination of medical guidance, lifestyle changes, and adherence to prescribed medications. The use of Contrave and Ozempic together may provide an effective tool for some, but only when used responsibly under medical supervision.
Deciding if Contrave is Right for You: Eligibility, Risks, and Benefits
Introduction
Contrave is a prescription weight loss medication that combines two active ingredients—bupropion and naltrexone—to support weight management by targeting appetite and cravings. Designed for adults struggling with obesity or weight-related health conditions, Contrave works as part of a broader approach involving diet and exercise.
Deciding if Contrave is right for you depends on individual eligibility, health history, and the potential benefits it may offer. Understanding these factors is essential for safe and effective weight loss. This article explores questions about what Contrave is, who it’s best suited for, and the advantages and considerations of using this medication.
Key Takeaways
- Contrave combines bupropion and naltrexone to suppress appetite and manage cravings.
- It is intended for adults with a BMI of 30+ or 27+ with weight-related health conditions.
- Consulting with a healthcare provider is critical to determine eligibility and ensure safety.
What is Contrave? An Overview
Contrave is a prescription medication approved by the FDA in 2014 to assist with weight loss in compatible adults who meet specific criteria. It contains two active components: bupropion, an antidepressant that also reduces appetite, and naltrexone, a drug used to treat addiction that may curb cravings. Together, these ingredients influence areas of the brain associated with hunger and reward, helping users achieve weight loss goals more effectively.
Unlike stimulant-based weight loss drugs, Contrave operates without affecting the central nervous system in the same way, making it a potential option for those who cannot tolerate stimulants. It is designed to be used alongside a reduced-calorie diet and increased physical activity to optimize results. Contrave’s dual-action approach differentiates it from other medications, offering an alternative for individuals struggling to control both appetite and cravings.
Eligibility Criteria for Contrave
BMI Requirements
Contrave is prescribed for a subset of adults with a body mass index (BMI) of 30 or higher, classifying them as obese. It is also an option for those with a BMI of 27 or higher if they have weight-related health conditions such as type 2 diabetes, high blood pressure, or high cholesterol. These criteria ensure the medication is targeted at individuals who may benefit most from its weight-loss properties.
Health Conditions
Candidates for Contrave often have weight-related health concerns that may improve with weight loss. Conditions such as insulin resistance, sleep apnea, and metabolic syndrome can make it difficult to lose weight without medical assistance. Contrave is part of a comprehensive plan to address these challenges.
Who Should Avoid Contrave
Certain individuals should not use Contrave due to safety concerns. It is contraindicated for:
- Pregnant or breastfeeding individuals.
- Those with seizure disorders or a history of seizures, as bupropion may increase seizure risk.
- Individuals taking opioids, which can interact negatively with naltrexone.
- People with uncontrolled hypertension or eating disorders such as bulimia or anorexia.
Consulting with a healthcare provider is essential to determine if Contrave is appropriate based on medical history, current medications, and overall health.
Benefits of Contrave
Contrave weight loss benefits are many, including the following:
Weight Loss Support
Contrave targets two significant barriers to weight loss: appetite and cravings. By suppressing hunger signals and reducing the urge to overeat, it can help individuals adhere to a calorie-controlled diet. This dual action supports gradual, sustained weight loss when combined with lifestyle changes.
Health Improvements
Weight loss achieved with Contrave may contribute to improved health outcomes, such as lower blood pressure, better blood sugar control, and reduced cholesterol levels. These changes can decrease the risk of developing chronic diseases like heart disease or type 2 diabetes, providing long-term health benefits.
Quality of Life
Losing weight can also enhance quality of life by increasing energy levels, improving mobility, and boosting self-esteem. Many users report feeling more confident and capable of engaging in physical activities they previously avoided.
Best Results with Lifestyle Changes
Contrave works most effectively when paired with a healthy diet and regular physical activity. For example, incorporating nutrient-dense foods and consistent exercise can enhance weight loss outcomes while promoting overall wellness. This comprehensive approach ensures the medication complements, rather than replaces, a healthy lifestyle.
Deciding if Contrave is Right for You: Risks and Considerations
Side Effects
Like all medications, Contrave comes with potential side effects. Common issues include nausea, headache, dizziness, constipation, and dry mouth, which often diminish as the body adjusts to the medication. More serious side effects, such as high blood pressure, seizures, or changes in mood, require immediate medical attention. Discussing potential side effects with a healthcare provider can help individuals prepare for what to expect.
Lifestyle Adjustments
Taking Contrave requires commitment to a healthier lifestyle. While the medication can help suppress appetite and control cravings, long-term success depends on adopting sustainable habits, such as eating a balanced diet and staying physically active. Consistency in these areas is key to achieving and maintaining weight loss.
Ongoing Monitoring
Regular check-ins with a healthcare provider are essential for monitoring progress and addressing any concerns. These appointments allow for adjustments to the treatment plan if necessary, ensuring the medication is used safely and effectively. Regular check-ins with a healthcare provider are essential for monitoring progress and addressing any concerns. If you’re still wondering, ‘Is Contrave right for you’, consulting with your doctor can help you decide.
Financial Considerations
The cost of Contrave can be a barrier for some individuals. While insurance may cover the medication, coverage varies, and out-of-pocket expenses can be significant. Exploring discount programs or manufacturer coupons can help reduce costs. Consulting with a pharmacist or insurance provider can clarify coverage options.
Drug Interactions
Contrave is known to interact with more than 700 drugs. Contrave and Wellbutrin drug interactions are particularly troubling, as are Contrave and Phentermine drug interactions. Though less researched, Contrave and Ozempic together drug interactions also exist. Always tell your healthcare provider all of the other medications you’re taking prior to starting Contrave.
Frequently Asked Questions About Contrave
- Who is the ideal candidate for Contrave?
Contrave is recommended for adults with a BMI of 30 or higher or a BMI of 27 or higher with at least one weight-related condition, such as type 2 diabetes or hypertension. Candidates should be willing to commit to lifestyle changes like a healthy diet and regular exercise. A healthcare provider will evaluate individual medical histories and medications to determine if Contrave is a suitable option. - Can Contrave be taken long-term?
Contrave is intended for use over an extended period, provided it continues to support weight loss and the individual tolerates it well. Healthcare providers typically assess progress after 12 to 16 weeks to determine whether to continue treatment. If significant weight loss has not occurred, the provider may recommend discontinuing the medication. - What lifestyle changes are necessary when taking Contrave?
To achieve the best results, users should adopt a reduced-calorie diet and engage in regular physical activity. These changes help maximize weight loss and improve overall health. Additionally, individuals should focus on building sustainable habits, such as meal planning and incorporating movement into daily routines, to maintain progress after stopping the medication. - Does Contrave work for everyone?
While Contrave has been shown to aid weight loss for many users, it may not work for everyone. Factors such as adherence to lifestyle changes, individual metabolism, and response to the medication can affect outcomes. Regular consultations with a healthcare provider help determine whether Contrave is effective or if adjustments are needed. - Is Contrave covered by insurance or discount programs?
Insurance coverage for Contrave varies depending on the provider and individual plan. Many insurers require prior authorization or proof of medical necessity before covering the medication. For those without insurance coverage, manufacturer coupons and savings programs may lower the cost. Checking with a pharmacist or insurance representative can clarify available options.
Conclusion
Contrave offers a potential solution for adults struggling with weight management, particularly those who meet specific eligibility criteria and are committed to making lifestyle changes. Understanding its benefits, risks, and requirements ensures informed decision-making. Always consult a healthcare provider to determine if Contrave aligns with your health needs and goals. Sustainable weight loss relies not just on medication but also on a commitment to healthier habits.