Contrave and Methadone Drug Interactions: A Risky Combo?

Combining medications can sometimes provide powerful therapeutic benefits. Other times, it can pose serious risks. For individuals prescribed both Contrave and methadone, understanding the potential for interaction is not just helpful—it’s essential.
Both drugs serve important roles in treating specific conditions: Contrave is commonly prescribed for weight loss, while methadone is widely used in treating opioid addiction and managing chronic pain. But using them together can carry important safety concerns.
This article provides a medically accurate, clear-eyed look at Contrave and methadone drug interactions, highlighting when the combination might be helpful, when it might be harmful, and what to discuss with your healthcare provider.
Key Takeaways
- Contrave and methadone can affect each other’s impact on the brain and body, increasing the risk of side effects such as seizures, blood pressure spikes, and respiratory depression.
- Patients with a history of drug addiction, bipolar disorder, or uncontrolled high blood pressure may be at especially high risk when combining these medications.
- Always talk with your doctor or healthcare provider before combining any medication, especially those that affect the central nervous system.
Understanding Contrave and Methadone
What is Contrave?
Contrave is a prescription medication approved for weight loss in certain adults who are at risk of a weight-related medical condition, such as type 2 diabetes or high blood pressure. It’s a drug combination made up of bupropion and naltrexone. Bupropion is also used to treat depression, quit smoking, and reduce cravings. Naltrexone is typically used to treat opioid addiction and alcohol use disorder.
Together, these components help decrease appetite and reduce food cravings, especially when combined with a reduced-calorie diet and increased physical activity to help compatible patients lose weight and manage weight long-term.
What is Methadone?
Methadone is a narcotic medicine used primarily in the treatment of opioid addiction and chronic pain. It works by altering how the brain and nervous system respond to pain.
Methadone is also used to prevent withdrawal symptoms in people who have become dependent on other street drugs, such as heroin.
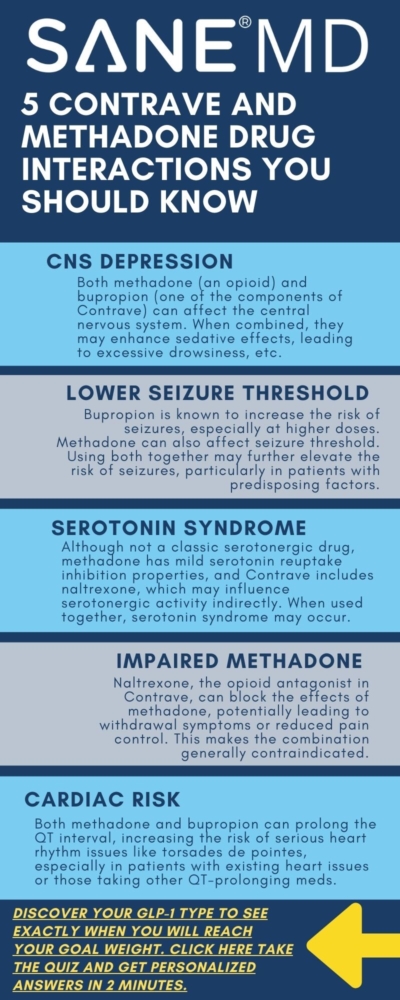
How Contrave and Methadone May Interact
When taken together, Contrave and methadone can result in complex and sometimes dangerous drug interactions, primarily due to the way both affect the brain and central nervous system. Contrave contains bupropion, an atypical antidepressant that also helps certain patients lose weight by suppressing appetite and cravings. Methadone, on the other hand, is a long-acting narcotic medicine that binds to opioid receptors to manage pain or treat opioid addiction.
Bupropion has a well-documented association with increased risk of seizures, particularly at higher doses or in patients with predisposing factors such as eating disorders, head injury, or use of other drugs that lower the seizure threshold, such as alcohol and caffeine. Methadone itself, while not commonly linked to seizures, can cause respiratory depression, sedation, and changes in brain chemistry that may further increase the risk when used in combination.
In addition to the seizure risk, Contrave’s naltrexone component can block opioid receptors. This means that it can reduce or completely negate the effectiveness of methadone, especially in people using methadone for opioid withdrawal or maintenance therapy.
This antagonistic effect can lead to sudden withdrawal symptoms, some of which may require emergency medical attention.
“One of the most concerning risks when combining bupropion and methadone is seizure susceptibility,” explains Dr. Matthew Olesiak, MD, Chief Medical Director at SANE MD. “Methadone alters neurotransmitter levels in the brain, and bupropion may further increase the risk of seizures, especially in individuals with other predisposing factors.”
The interaction becomes even more unpredictable when factoring in other medications a patient might be taking, such as seizure medication, over-the-counter drugs, or antidepressant medicine.
The combined CNS (central nervous system) effects can result in heightened sedation, increased risk of confusion, or erratic mood swings.
Possible Side Effects and Risks
The combination of Contrave and methadone can affect multiple systems in the body, particularly the neurological, cardiovascular, and gastrointestinal systems.
Side effects may be mild in some individuals, but they can also escalate quickly without warning.
Seizures
This is one of the most dangerous risks associated with this drug combination. Bupropion may increase the risk of seizures, especially in patients with a history of head injury, eating disorder, or those taking other medicines that interact with the brain.
Methadone could intensify these effects by disrupting normal brain activity and causing fluctuations in neurotransmitter levels.
Increased blood pressure or uncontrolled high blood pressure
Both medications can raise blood pressure, especially bupropion.
When combined, the risk of developing uncontrolled high blood pressure grows significantly, particularly if patients are also consuming high-fat meals, drinking alcohol, or have a history of hypertension. Our comprehensive guide details how Contrave can increase blood pressure.
Respiratory depression
Methadone is a powerful narcotic medicine that can slow breathing.
If taken in conjunction with other CNS depressants or medications like bupropion, which have stimulating effects, the interaction can be unpredictable—resulting in dangerously slow breathing or sudden apnea in high-risk individuals.
Blurred vision
Changes in vision, such as blurred vision or even eye pain, have been reported in some users of both drugs.
This may be a sign of increased intracranial pressure or other neurological effects and should be addressed promptly.
Dry mouth, stomach pain, or joint pain
These symptoms, while more common and typically less dangerous, may still signal that the body is struggling to metabolize the drug combination effectively.
Persistent stomach pain or joint pain should prompt a consultation with a healthcare provider.
Suicidal thoughts or panic attacks
Patients with underlying mood disorders or taking these drugs to treat depression may experience worsening symptoms.
The risk of suicidal thoughts, panic attacks, and emotional volatility may be increased when Contrave and methadone are used together, especially without careful psychiatric monitoring.
Opioid withdrawal symptoms
Since Contrave includes naltrexone, it can block the effects of methadone.
This blocking can trigger acute opioid withdrawal, with symptoms ranging from agitation and nausea to chest pain, trouble sleeping, and even seizures.
Skin rash, serious skin reactions, or severe skin reaction
Rare, but serious, skin reactions have been linked to both medications.
If a skin rash develops—especially when accompanied by fever, dark urine, or mucosal swelling—it may be a sign of a severe skin reaction requiring immediate medical attention.
Dark urine or eye pain
These may indicate liver strain or neurological side effects and should be reported to your healthcare provider right away.
In rare cases, this combination could lead to a dangerous drug interaction. Since methadone is a full opioid agonist and naltrexone is an opioid antagonist, their effects can directly oppose each other.
This may trigger opioid withdrawal symptoms, especially in patients who are actively dependent on methadone for addiction therapy.
“Naltrexone can block the effects of opioids,” Dr. Olesiak notes. “If someone is taking methadone and starts Contrave without medical guidance, they may experience opioid withdrawal that can be intense and even dangerous. Always talk with your doctor before starting or stopping any medication.”
Who Is at Higher Risk?
1. Individuals with Pre-existing Conditions
People with kidney disease, bipolar disorder, head injury, or an eating disorder may be at greater risk for adverse effects.
For example:
- A person with kidney disease may have trouble clearing the drugs from their body, raising the risk of toxicity.
- Those with bipolar disorder may experience manic episodes triggered by bupropion’s stimulant-like properties.
- Individuals with an eating disorder or history of drug addiction already face a higher risk of seizures, especially when combining CNS-active drugs like Contrave and methadone.
2. People with Mental Health Conditions
Mental health conditions like depression, anxiety, or past trauma can worsen when taking medications that alter mood and brain chemistry. Contrave has been associated with suicidal thoughts, especially in people taking it to treat depression.
Combining it with methadone, especially in those also using antidepressant medicine or seizure medication, may lead to unpredictable mood swings, new or worsening symptoms, and unusual risk-taking behavior.
Even patients in recovery from addiction may relapse or feel destabilized due to the contrasting effects of methadone (which reduces cravings) and naltrexone (which blocks opioids entirely).
3. Patients Taking Other Medications
If you are taking other medicines—especially over-the-counter drugs, weight loss products, or prescription diet pills—you should be extremely cautious. Many over-the-counter medicines for cold symptoms, sleep aids, or pain relief may interact with the central nervous system, amplifying side effects or interfering with drug metabolism.
In addition, patients who drink alcohol regularly may further increase their risk of liver strain, chest pain, serious allergic reactions, or trouble sleeping. Alcohol, methadone, and bupropion all affect brain activity, and combining them could be dangerous.
According to the FDA, combining methadone with CNS depressants—including alcohol and certain medications—can increase the risk of slowed breathing, overdose, and death, and should be managed with extreme caution by healthcare providers. [FDA Drug Safety Communication, 2017]

Warning Signs to Watch For
If you’re taking both medications, it’s essential to monitor for warning signs that may indicate a serious reaction.
Seek emergency medical attention or immediate medical attention if you experience:
- Sudden chest pain
- Severe stomach pain or eye pain
- Signs of a serious allergic reaction (such as swelling of the face, tongue, or throat)
- A severe skin rash or serious skin reaction
- Dark urine, yellowing of the eyes or skin
- Increased blood pressure or symptoms of high blood pressure (like pounding headaches or dizziness)
- Confusion, hallucinations, or panic attacks
Safety Measures and Alternatives
When considering any combination therapy—especially involving medications like Contrave and methadone—it’s essential to take proactive safety steps.
Not everyone will experience side effects, but for those at risk, having safeguards in place can prevent serious complications.
The goal is not just to lose weight or manage pain but to do so safely under the supervision of a trusted healthcare provider.
Talk With Your Doctor
Before starting, stopping, or combining medications, talk with your doctor.
Both Contrave and methadone come with complex pharmacological profiles, and their interaction can result in anything from mild side effects to a dangerous drug interaction.
You should tell your doctor if you:
- Have a personal or family history of seizures, epilepsy, or other neurological disorders. Bupropion, a component of Contrave, is known to increase the risk of seizures, and that risk may be amplified if methadone is added to the mix.
- Are being treated for or have a history of mental illness, including bipolar disorder, panic attacks, or suicidal thoughts. Your provider may need to adjust your treatment plan or monitor you more closely.
- Are pregnant, trying to conceive, or breastfeeding. Both medications have potential implications for your unborn baby, including withdrawal symptoms and developmental risks. Discuss potential alternatives or timing strategies with your healthcare provider.
- Drink alcohol regularly or use street drugs or other street drugs. Alcohol and illicit substances can dramatically increase the risk of side effects like chest pain, confusion, or serious allergic reactions, and interfere with both methadone and Contrave.
- Are using diet pills, supplements, or over-the-counter products. Many of these contain stimulants, depressants, or other compounds that may worsen drug interactions.
- Have weight-related medical problems such as high blood pressure, low blood sugar, or blood sugar instability. These may be affected by changes in appetite, metabolism, or mood caused by either medication.
It’s critical to also disclose whether you are using medications for other conditions—especially seizure medications, heart medications, antidepressant medicines, or any over-the-counter medicines for sleep, pain, or allergies. Certain medicines can increase sedation, spike blood pressure, or alter how your liver processes Contrave or methadone.
When in doubt, bring your prescription label, supplement bottles, or even a written list of everything you’re taking to your appointment. Your provider can help identify possible interactions, and the more they know, the safer your treatment plan will be.
Medication Guide and Dosing
Your safety also depends on how carefully you follow your prescribed treatment plan. Always read the full medication guide that comes with each prescription, even if you’ve taken the medication before. These guides are updated regularly to reflect new warnings, dosing changes, and safety notices.
Here are key tips for dosing:
- Follow your doctor’s dosing instructions exactly. Don’t self-adjust your dose to “speed up” weight loss or enhance pain relief. Doing so could increase your risk of seizures, low blood sugar, or respiratory depression.
- Take each medication at the same time each day (if instructed), and avoid combining them with high-fat meals, which can intensify side effects like nausea or blurred vision.
- If you miss a dose, don’t take two at once. Doubling up on a missed dose can lead to serious issues like stomach pain, confusion, or increased blood pressure.
- Avoid stopping either drug abruptly, especially methadone. Discontinuing without tapering may lead to opioid withdrawal, trouble sleeping, or mood disturbances.
Considering Safer Alternatives
If you’re concerned about the risks, there may be alternatives.
Your healthcare provider might recommend:
- Trying a different weight loss medication that doesn’t include naltrexone, especially if you are dependent on opioids or in recovery.
- Prioritizing non-drug approaches like a reduced-calorie diet, physical activity, and behavioral therapy.
- Adjusting methadone doses gradually if your long-term plan includes Contrave, under close supervision.
- Exploring different therapies for opioid addiction, such as buprenorphine, that may carry less risk when paired with Contrave or weight loss products.
Every treatment plan should be individualized. There’s no one-size-fits-all solution when managing chronic conditions like obesity and addiction—but there is a path that minimizes harm and maximizes benefit. It starts with open communication and informed choices.
Can You Still Use Contrave If You’re on Methadone?
It depends. In some cases, healthcare providers may cautiously prescribe Contrave to patients on methadone.
However, this requires careful monitoring, dosage adjustments, and regular checkups. Indeed, the FDA’s labeling information states that methadone and other opioid agonists or partial agonists are contraindicated for use with Contrave.
Your healthcare provider may suggest:
- Adjusting the Contrave dose or using an alternative weight loss medication
- Delaying Contrave use until methadone is tapered or discontinued
- Exploring lifestyle-based strategies such as a reduced-calorie diet and exercise
- Checking blood pressure regularly, especially if you have uncontrolled high blood pressure
- Testing blood sugar levels to prevent episodes of low blood sugar
Final Reminders
- Don’t stop or start medications without professional guidance.
- Follow your prescription label and read the medication guide closely.
- Tell your doctor about any supplements, over-the-counter drugs, or other medicines you’re taking.
- If you experience chest pain, eye pain, serious skin reactions, or dark urine, seek emergency medical attention right away.
While not everyone will experience issues from taking these two medications together, being informed—and having regular conversations with your healthcare provider—is the best way to stay safe.
Frequently Asked Questions (FAQ)
If you’re considering Contrave for weight loss while taking methadone—or vice versa—you likely have questions about potential drug interactions and safety concerns.
Below are answers to some of the most common questions patients ask. Remember, this information is not a substitute for medical advice. Always talk with your doctor or healthcare provider before making changes to your treatment plan.
1. Can you take Contrave with methadone?
In some cases, healthcare providers may prescribe Contrave and methadone together, but this combination carries significant risks and requires close medical supervision. The main concern is that naltrexone, one of the active ingredients in Contrave, can block the effects of methadone, potentially triggering opioid withdrawal symptoms.
Additionally, bupropion in Contrave may increase the risk of seizures, especially when combined with other drugs that affect the central nervous system. If you’re using methadone to manage opioid addiction or chronic pain, talk with your doctor before starting Contrave.
2. Can you take bupropion and methadone together?
While it is sometimes done under supervision, combining bupropion and methadone can raise safety concerns. Bupropion is known to lower the seizure threshold and may increase the risk of seizures, particularly in people with other risk factors like head injury, eating disorder, or use of additional CNS-active drugs. Methadone also impacts brain chemistry, which can intensify this effect.
If a healthcare provider decides to prescribe both, they will likely monitor you closely for side effects such as mood changes, trouble sleeping, or neurological symptoms. Always tell your doctor about all medications you’re taking.
3. Can you take opioids on Contrave?
No, taking opioids while on Contrave is not recommended and can be dangerous. Contrave contains naltrexone, an opioid receptor antagonist, which blocks the effects of opioids. This means opioids will be less effective or completely ineffective for pain relief or recreational use. Attempting to overcome this blocking effect by taking more opioids can lead to overdose and serious side effects, including respiratory depression and chest pain.
Always talk with your doctor if you need opioid medication for any reason while taking Contrave.
4. What medications should I avoid with Contrave?
Several other medicines can interact with Contrave and should be used cautiously or avoided altogether. These include opioids (Codeine, Oxycodone), seizure medication (Topamax), antidepressant medicine (Effexor, Lexapro), especially MAOI medications (Nardil), certain over-the-counter cold and allergy products (Benadryl), and other weight loss products (Mounjaro) or diet pills (Phentermine, Qsymia). Combining Contrave with these drugs may increase the risk of side effects such as high blood pressure, seizures, or serious skin reactions.
Also, avoid high-fat meals, which can affect how the drug is absorbed and may worsen nausea. To stay safe, tell your doctor about every medication, supplement, or herb you use, even if it seems minor.
5. What happens if you take opioids with Contrave?
Taking opioids while on Contrave can result in opioid withdrawal, which may come on suddenly and be quite severe. This happens because Contrave contains naltrexone, which blocks the opioid receptors in your brain and prevents opioids from working.
Symptoms of withdrawal may include nausea, vomiting, sweating, anxiety, stomach pain, and agitation. In some cases, it may lead to medical emergencies that require immediate medical attention.
If you’re prescribed opioid painkillers or are in recovery from opioid use, be sure to talk with your doctor before starting or continuing Contrave.
Conclusion
The combination of Contrave and methadone can be a risky combo, particularly if prescribed without full oversight. Although both drugs have unique benefits—one supporting weight loss, the other helping to treat opioid addiction—the potential for drug interactions is real and must be taken seriously.
Always work closely with your healthcare provider, especially if you’re prescribed other medicines or have underlying health conditions. Let your provider know if you experience trouble sleeping, low blood sugar, blurred vision, or suicidal thoughts. The goal is safe, effective treatment—not unexpected harm.
“Patients often assume that if medications are prescribed separately, they must be safe together,” says Dr. Olesiak. “But that’s not always the case. These two drugs can interact in unpredictable ways, and talking with your doctor is the safest way to avoid a dangerous drug interaction.”
References
FDA Contrave Labeling/Prescribing Guidelines

Contrave and Ephedrine Drug Interactions Guide

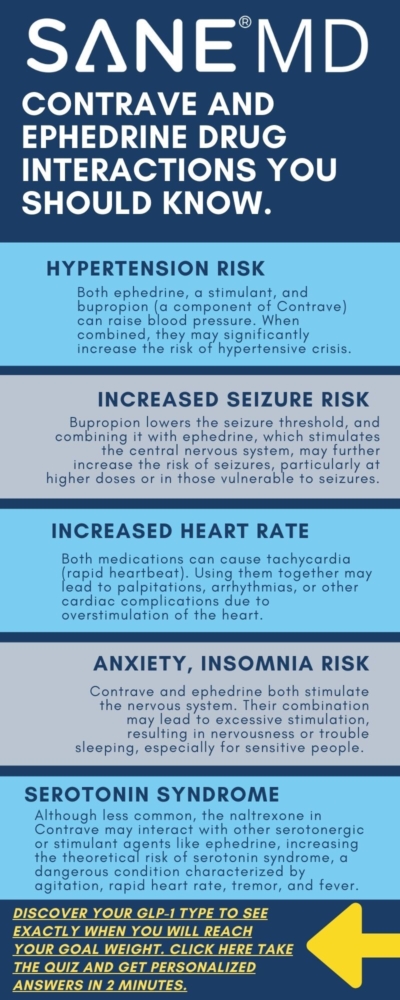
Combining weight loss medications like Contrave with stimulant compounds such as ephedrine may sound like a shortcut to faster results, but the potential for serious drug interactions cannot be overstated. Both medications influence the central nervous and cardiovascular systems, raising significant concerns when taken together. Understanding how these compounds interact is crucial for anyone looking to lose weight safely and effectively.
In this guide, we’ll explore how Contrave and ephedrine work individually, how they may interact, and why caution is strongly advised. We’ll also cover side effects, risks, and alternatives for those seeking weight loss medications with fewer complications. By the end of this article, you should have a solid understanding of Contrave and Ephedrine drug interactions.
Key Takeaways
- Combining Contrave and ephedrine can dangerously elevate blood pressure and heart rate, increasing the risk of cardiovascular events.
- Both compounds act as appetite suppressants, but their overlapping effects on the central nervous system heighten the chance of adverse effects.
- Safer, evidence-based prescription drugs and lifestyle changes are recommended over unregulated dietary supplements containing ephedrine.
What Is Contrave and What Is It Used For?
Contrave is a combination medication composed of bupropion and naltrexone, both of which are FDA-approved and prescribed for weight loss in certain adults with a body mass index (BMI) of 30 or more—or 27 with an obesity-related condition like type 2 diabetes or high cholesterol. Contrave is classified as one of several available weight loss medications that work by targeting the brain’s appetite and reward centers.
Bupropion is also used to treat depression and help people stop smoking, while naltrexone is commonly prescribed to treat alcohol and drug dependence. Together, they form an appetite suppressant designed to help compatible patients reduce food intake and lose weight over time.
“Contrave has shown efficacy in reducing cravings and promoting gradual weight loss,” explains Dr. Matthew Olesiak, MD, Chief Medical Director at SANE MD. “But combining it with stimulants like ephedrine is dangerous and not supported by clinical data.”
Contrave is not a controlled substance, but because bupropion affects dopamine levels, misuse or abuse can occur. Doctors often avoid prescribing it to individuals with a personal or family history of drug dependence, eating disorder, or psychiatric symptoms.
What Is Ephedrine?
Ephedrine is a central nervous system stimulant found in many nonprescription diet pills and formerly popular formulations like the Brazilian diet pill. Due to its appetite suppressant properties, it was once widely used in over-the-counter cold medicines and weight loss aids.
Ephedrine stimulates the heart and increases blood pressure and heart rate. While it can reduce food intake and boost metabolism temporarily, it is linked to dangerous side effects, including:
- High blood pressure
- Chest pain
- Stomach upset
- Migraine headaches
- Severe cardiovascular events
Because of its serious risks, especially in those with uncontrolled high blood pressure, coronary heart disease, or heart disease, the Food and Drug Administration banned ephedrine-containing dietary supplements in 2004. However, it is still found in some recommended dietary supplements purchased internationally or online.
“Patients often underestimate the risks of ephedrine because it’s marketed as a natural solution,” warns Dr. Olesiak. “But it’s a potent stimulant that can lead to dangerous interactions when combined with prescription drugs like Contrave.”
Contrave and Ephedrine Drug Interactions Summary Table
| Category | Contrave | Ephedrine | Interaction Concern |
|---|---|---|---|
| Drug Class | Combination of bupropion (antidepressant) and naltrexone (opioid antagonist) | Sympathomimetic stimulant (acts on adrenergic receptors) | Both act on the central nervous system, leading to overlapping stimulant effects |
| Primary Use | Prescription weight loss medication for obesity management | Formerly used in appetite suppressant products; still present in some supplements | Concurrent use is unapproved and increases health risks |
| Mechanism of Action | Reduces cravings and food intake by altering dopamine/norepinephrine | Increases heart rate and reduces appetite by stimulating the CNS | Overstimulation can occur, increasing the risk of side effects |
| Effects on Blood Pressure | May increase blood pressure in some users | Known to cause high blood pressure and heart rate elevation | Additive effect may cause dangerously elevated blood pressure |
| Seizure Risk | Bupropion lowers seizure threshold | Can increase CNS excitability | Combined use significantly raises seizure risk |
| Psychiatric Symptoms | Possible anxiety, agitation, mood swings | Can cause nervousness, insomnia, and anxiety | Combined stimulation may lead to psychiatric symptoms |
| Heart-Related Risks | Caution in patients with heart disease or arrhythmia history | Can cause chest pain, arrhythmia, and palpitations | Increased risk of cardiovascular events, especially in predisposed individuals |
| Drug Interaction Classification | Moderate to Major Risk | Moderate to Major Risk | Not recommended; use together only under strict medical supervision (generally discouraged) |
| FDA Status | FDA-approved prescription drug | Banned in U.S. dietary supplements by the FDA | Combining a regulated prescription with an unregulated compound increases unpredictability |
| Clinical Recommendation | Safe when used alone under supervision | Unsafe in many cases; banned in supplement form | Do not combine; opt for FDA-approved weight loss drugs or alternatives recommended by a physician |
Contrave and Ephedrine Drug Interactions: Why They Don’t Mix
Combining Contrave and ephedrine is strongly discouraged due to the potential for serious drug interactions. Both compounds influence the central nervous system and cardiovascular system, and when taken together, they can significantly magnify each other’s effects.
This increases the likelihood of harmful outcomes such as:
- Heart palpitations
- Elevated blood pressure
- Abnormal heart rhythm
- Chest pain
- Seizures
- Psychiatric symptoms
These effects are not just theoretical. They reflect real pharmacological interactions that place excessive strain on the heart, brain, and metabolic systems, especially in individuals using the combination to lose weight quickly without medical guidance.
Cardiovascular Stress
One of the most alarming risks of combining these drugs is the additive stress on the cardiovascular system. Ephedrine, a stimulant once common in many nonprescription diet pills, increases blood pressure, accelerates the heart rate, and constricts blood vessels.
Meanwhile, bupropion, a key component in Contrave, can also cause increased blood pressure in certain users—particularly at higher doses or when combined with other medications that stimulate the nervous system.
Together, these drugs can cause a dangerous spike in blood pressure and even trigger cardiovascular events such as arrhythmias, chest pain, or, in extreme cases, stroke or heart attack. This is particularly hazardous for patients with:
- High blood pressure
- Coronary heart disease
- Cardiovascular disease
- High cholesterol
- A family history of heart conditions
Because of the overlapping cardiovascular effects, this combination is considered high risk and should be avoided even in individuals without pre-existing heart conditions.
Neurological Risks
The neurological overlap is equally concerning. Both Contrave and ephedrine act as appetite suppressants by stimulating the brain’s neurotransmitters, particularly dopamine and norepinephrine. While this mechanism helps reduce food intake and facilitate weight loss, it also puts users at risk for severe side effects when overactivated.
Bupropion is already known to lower the seizure threshold, making seizures more likely, especially in those with a personal or family history of seizure disorders or those taking high-fat meals, which increase bupropion absorption. Introducing ephedrine into the system further elevates seizure risk, as it is also a central nervous stimulant that can exacerbate nervous system excitability.
This interaction becomes especially dangerous for patients with a history of:
- Eating disorder
- Alcohol and drug dependence
- Drug abuse
- Migraine headaches
- Psychiatric symptoms like anxiety, agitation, or mania
Combining the two increases the likelihood of adverse effects such as insomnia, panic attacks, and in extreme cases, psychosis or dangerous behavior changes.
Appetite Suppression Overlap
Contrave and ephedrine are both designed to reduce food intake—but suppressing appetite too aggressively can backfire. A significant reduction in hunger may lead to a sharp decline in nutrient consumption, placing the body in a near-starvation state. (The same risk can occur when combining Contrave and Phentermine, another appetite-suppressing drug.
While this can lead to initial weight loss, it may also cause:
- Stomach cramps
- Abdominal pain
- Fatigue
- Stomach upset
- Electrolyte imbalances
- Hormonal disruption
- Increased liver strain
In rare cases, rapid body weight loss combined with poor nutrition can trigger severe liver injury or other organ complications. Individuals with a low body mass index or those already on a very low-calorie diet are especially vulnerable. For long-term success, it’s important to aim for maintained weight loss supported by safe, sustainable methods—not aggressive chemical suppression of appetite at the cost of health.
Potential Side Effects When Combining Contrave and Ephedrine
The side effects of each medication are concerning on their own, but when used together, their impact can be amplified and lead to unpredictable reactions in the body.
Some of the most frequently reported or anticipated adverse effects include:
- High blood pressure
- Increased heart rate
- Abdominal pain
- Chest pain
- Severe headaches
- Stomach upset
- Insomnia
- Seizures
- Anxiety
- Nausea
- Dizziness
- Psychiatric symptoms such as agitation, mood swings, or paranoia
These reactions are not limited to physical discomfort; they can also worsen underlying mental health conditions or create new psychiatric complications. For individuals with drug dependence histories, combining Contrave with ephedrine may reawaken cravings or cause emotional instability.
Furthermore, individuals with pre-existing liver problems or those taking other medications that affect liver enzymes (such as certain diabetes medications or antidepressants) may be at higher risk of severe liver injury due to increased metabolic demand.
Some users may experience rare but significant complications, including:
- Signs of medullary thyroid cancer (linked to other weight loss drugs like GLP-1 agonists)
- Hormonal imbalances that may affect thyroid function or blood sugar
- Unexpected weight fluctuations, especially weight gain after stopping stimulants
Because Contrave and ephedrine drug interactions affect multiple organ systems—heart, brain, liver, and endocrine—any attempt to combine them should be under strict medical supervision (though generally it’s advised not to combine them at all).
The Food and Drug Administration has issued multiple advisories regarding the risks of combining stimulants and prescription drugs that affect the brain and cardiovascular system.
Alternatives to Ephedrine and Safer Weight Loss Strategies
Fortunately, there are safer weight loss medications on the market with better safety profiles and clinical backing.
These include:
- GLP-1 agonists like semaglutide (Ozempic), which promote satiety and reduce food intake
- Diabetes medications that also help control blood sugar levels and reduce body weight
- Lifestyle changes such as a low-calorie diet, exercise, and behavioral support
- FDA-approved drugs like phentermine-topiramate (Qsymia) or orlistat, which are better understood in terms of long-term safety data
Keep in mind that you still should not combine any of the above medical alternatives with Contrave without consulting your healthcare providers, as many of them, such as Qsymia, can interact with Contrave.
Some individuals consider bariatric surgery or weight loss procedures, especially if their body mass index is above 40 or if they have obesity-related complications.
“When paired with behavior modification and nutritional support, FDA-approved medications provide a more sustainable path to weight loss,” says Dr. Olesiak. “Quick fixes like ephedrine are neither safe nor effective long term.”
Understanding the Role of Contrave
Contrave is a combination medication made of bupropion and naltrexone, both of which have been independently used for decades. When combined, they offer a dual mechanism to promote weight loss by targeting hunger signals and reward-driven eating in the brain. As a prescription weight loss aid, Contrave is designed for certain adults with a body mass index (BMI) of 30 or greater, or 27 and above with conditions such as high blood pressure, type 2 diabetes, or high cholesterol.
Contrave works primarily by affecting two key brain pathways: the hypothalamus, which regulates appetite and food intake, and the mesolimbic dopamine system, which drives cravings and reward-seeking behaviors. This makes it particularly effective for patients who struggle with emotional eating or binge-eating patterns.
Clinical research has demonstrated that Contrave can lead to average weight loss of 5% to 9% of a patient’s initial body weight over a 6 to 12-month period when used alongside lifestyle changes like reduced-calorie eating and increased physical activity.
“Contrave helps reduce cravings while also promoting a sense of fullness,” explains Dr. Matthew Olesiak, MD. “It’s an effective tool for many patients who haven’t responded well to other weight loss medicines.”
Contrave may be especially useful for people with:
- A history of emotional eating or binge episodes
- Prior or current alcohol and drug dependence
- Comorbid depression, as bupropion is also used to treat depression
- Previous failed attempts with other prescription drugs or available weight loss medications
However, despite its benefits, Contrave is not suitable for everyone. Many drugs and substances can interact with Contrave. Additionally, it should be avoided in people who have:
- Uncontrolled high blood pressure
- A seizure disorder or history of seizures
- An active eating disorder, such as bulimia or anorexia nervosa
- Current use of other bupropion-containing prescription drugs
- Dependence on opioids or undergoing opioid withdrawal
These contraindications are serious, as they raise the risk of side effects such as seizures, mood instability, or dangerously high blood pressure. Patients with a personal or family history of psychiatric or neurological disorders should be thoroughly evaluated before starting the medication.
Important Warnings When Using Contrave
Like all weight loss medications, Contrave carries specific precautions and usage guidelines to ensure safety and maximize its effectiveness. Understanding and following these warnings can help prevent adverse effects and improve treatment outcomes.
1. Avoid High-Fat Foods
Patients taking Contrave are advised to avoid high-fat foods—especially meals rich in saturated or trans fats—because they significantly increase the absorption of bupropion. This higher drug concentration can trigger more intense side effects, including nausea, headaches, dizziness, or even seizures in susceptible individuals.
A high-fat meal can also spike blood pressure and offset the balance of the medication.
2. Monitor Blood Pressure and Blood Sugar Closely
Because Contrave can raise blood pressure and heart rate in some users, regular monitoring is essential—especially for patients with a history of heart disease, diabetes, or those using other medications that may impact cardiovascular function or glucose control.
If you’re taking other diabetes medications or insulin, the dosage may need to be adjusted as body weight and blood sugar levels begin to change. Fluctuations in appetite or food intake may also affect how your body responds to these drugs.
3. Disclose All Dietary Supplements
Let your healthcare provider know about any dietary supplements you’re using—especially those advertised as an appetite suppressant or labeled to prevent weight gain. Some recommended dietary supplements, including those marketed as natural or herbal (like those containing green tea, herbathin dietary supplement, or caffeine), may interfere with Contrave’s absorption or effectiveness.
Unregulated supplements may also contain stimulants or hidden ingredients like ephedrine, which can result in dangerous drug interactions, increased side effects, or elevated blood pressure.
“Patients often believe supplements are harmless, but some interact directly with prescription medications and raise serious safety concerns,” notes Dr. Olesiak. “Always disclose all products you’re taking—even if they’re over the counter.”
4. Review Your Medical History in Full
Before starting Contrave, patients should share any personal or family history of:
- Cardiovascular disease
- Psychiatric symptoms, including mood disorders or bipolar disorder
- Drug abuse or drug dependence
- Seizures
- Liver problems
These conditions may require dosage modifications or make Contrave an inappropriate choice altogether. In rare cases, untreated psychiatric issues can worsen during treatment, and some patients may report new or increased psychiatric symptoms such as agitation, suicidal thoughts, or panic attacks.
Proper screening and ongoing evaluation are essential to minimize risks and ensure the safest experience possible with weight loss medicines like Contrave.

FAQ: Contrave and Ephedrine
Patients exploring weight loss medications often have questions about how different drugs and supplements may interact. Because both Contrave and ephedrine affect the central nervous system and cardiovascular system, it’s important to understand the risks of combining them—or using them alongside other compounds with similar mechanisms.
Below are answers to some of the most common questions related to these drug combinations.
1. Can you take bupropion and ephedrine together?
No, taking bupropion and ephedrine together is not recommended. Both drugs are stimulants and can significantly increase blood pressure, heart rate, and central nervous system activity. When combined, they raise the risk of dangerous side effects such as seizures, chest pain, anxiety, and even drug dependence.
Individuals with high blood pressure, a personal or family history of cardiovascular problems, or a seizure disorder face elevated risks from this combination. Always consult a healthcare provider before using either substance, especially in combination.
2. What medications should not be taken with Contrave?
Several prescription drugs and dietary supplements should not be taken with Contrave due to the risk of drug interactions. These include other medications that contain bupropion, monoamine oxidase inhibitors (MAOIs) such as Nardil, opioids, such as oxycodone or hydromorphone, and medications that lower the seizure threshold, such as certain antipsychotics and antidepressants.
Additionally, combining Contrave with appetite suppressant supplements or stimulants like ephedrine, pseudoephedrine, or high-dose caffeine can cause side effects such as insomnia, agitation, and dangerously high blood pressure. Patients should also avoid taking Contrave with a high-fat meal, which may increase drug absorption and adverse effects.
3. What not to mix with ephedrine?
Ephedrine should not be mixed with other stimulants, including bupropion, caffeine, pseudoephedrine, and some dietary supplements marketed as appetite suppressants. Combining ephedrine with these compounds can lead to cardiovascular disease, psychiatric symptoms, or dangerous spikes in blood pressure and heart rate. Ephedrine can also interact with prescription drugs used to treat depression or control blood sugar levels, increasing the risk of seizures and metabolic imbalance.
Anyone considering the use of ephedrine, even in over-the-counter products, should first review all current medications with a healthcare professional.
4. Can you take pseudoephedrine with Contrave?
Taking pseudoephedrine with Contrave is generally discouraged. Both substances can raise blood pressure and stimulate the cardiovascular system, increasing the risk of side effects such as rapid heart rate, insomnia, and nervousness. This combination is especially risky for individuals with uncontrolled high blood pressure, heart disease, or other medications that affect the nervous system.
While pseudoephedrine is commonly used for nasal congestion, safer alternatives may be recommended for patients currently using weight loss medications like Contrave.
5. Can you take bupropion and ephedrine together?
No, using bupropion and ephedrine together poses serious health risks and should be avoided. The combination increases the likelihood of seizures, psychiatric symptoms, and elevated blood pressure, especially in people with cardiovascular disease or a family history of heart issues.
Since both drugs act as appetite suppressants, they may also excessively reduce food intake, leading to fatigue or nutritional deficiencies. This pairing may also worsen the side effects of each drug, making the combination unsafe without direct medical supervision.
Final Thoughts
The use of Contrave alone can be a helpful tool to lose weight in individuals struggling with obesity, but combining it with ephedrine or other stimulants is a serious medical risk. While both may act as appetite suppressants, the overlap in their mechanisms of action significantly increases the likelihood of side effects—many of them dangerous.
Safer weight loss medicines, medically supervised programs, and lifestyle changes remain the most effective, evidence-based strategies for achieving and maintaining weight loss. Always consult a healthcare provider before combining weight loss drugs or using any dietary supplements marketed as appetite suppressants.

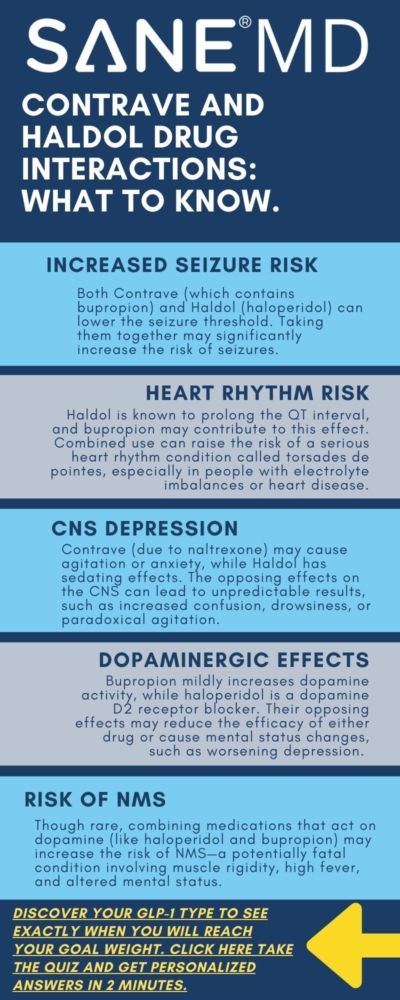
Contrave and Haldol Drug Interactions: What You Should Know

Combining medications can be life-changing—or life-threatening—depending on how the drugs interact in your body. This is especially true when using medications for weight loss or psychiatric conditions. One such combination, Contrave and Haldol, raises concerns about overlapping side effects, risks to mental stability, and the risk of seizures.
Understanding how these two medications affect one another is vital, particularly for patients managing both weight loss therapy and mental health disorders like bipolar disorder or major depressive disorder.
This article breaks down the potential Contrave and Haldol drug interactions, health concerns, and necessary precautions when taking Contrave and Haldol together.
Key Takeaways
- Taking Contrave with Haldol may increase the risk of serious side effects, including movement disorders, mental health changes, and a lowered seizure threshold.
- Patients with bipolar disorder, a seizure disorder, or other medical conditions must consult their doctor or pharmacist before combining these medications.
- Depending on your health history and treatment goals, the combination may require close monitoring, dosage adjustment, or even the use of other medications.
Understanding Contrave and Haldol
Contrave is a prescription medication specifically approved by the FDA for weight loss in certain adults who are overweight or obese and have a high initial body mass index (BMI ≥30, or ≥27 with comorbid conditions). The drug contains two active drugs: naltrexone hydrochloride, a drug class known as opioid antagonists, and bupropion hydrochloride, which belongs to a drug class of antidepressant drugs.
Bupropion hydrochloride is also found in other medications like Wellbutrin SR and Wellbutrin XL, used to treat depression and aid in smoking cessation. Meanwhile, naltrexone hydrochloride is known for its role in managing opioid withdrawal symptoms and alcohol dependence. Combined, these components help regulate brain pathways involved in appetite, cravings, and energy use. As part of a broader treatment plan that includes a reduced-calorie diet and increased exercise, Contrave treatment supports long-term weight loss and chronic weight management for compatible individuals.
However, taking Contrave requires careful oversight due to its potential to increase the risk of side effects, including high blood pressure, suicidal thoughts and behaviors, and a lowered seizure threshold. These risks can be magnified by certain drug interactions or underlying medical conditions, such as a history of seizure disorder, mental health instability, or liver impairment.
Haldol, or haloperidol, is a typical antipsychotic used for the treatment of psychiatric conditions, including schizophrenia, bipolar disorder, major depressive disorder with psychotic features, and acute psychosis. It alters chemical signals in the brain, primarily targeting the dopamine system, but it also affects the serotonergic neurotransmitter system. Haldol is often prescribed to manage severe agitation, delusions, hallucinations, and behavioral disturbances in psychiatric and medical patients.
While Haldol can be effective in stabilizing mental health, it is known for its potential to cause neurological side effects, including extrapyramidal symptoms (EPS), tardive dyskinesia, and, in rare cases, serotonin syndrome occurs when combined with other serotonergic agents. Because it is metabolized in the liver, it also poses concerns for those with severe hepatic impairment.
When used together, haloperidol bupropion interactions become clinically important. Taking Contrave alongside Haldol may lead to additive or synergistic effects on the seizure threshold, making it more likely that seizures will occur, especially in patients with risk factors such as a history of seizure disorder, mental health conditions, or who have suddenly stopped drinking alcohol.
Moreover, both drugs can affect blood pressure, the central nervous system, and emotional regulation, creating a scenario where side effects and adverse reactions must be closely monitored. The overlap in how these medications interact with the brain’s chemical messengers means that combining them can increase the risk of mental health changes, such as mood swings, irritability, or worsening depression.
Because of these risks, healthcare providers must consider the patient’s full health history, including other prescription drugs, over-the-counter drugs, and any ongoing medical conditions, before choosing to prescribe Contrave alongside Haldol.
Even though both medications are approved for their individual uses—one for weight loss and the other for mental health—their interaction represents a complex balance between benefit and harm. This is especially true when used in patients dealing with overlapping conditions such as bipolar disorder and obesity, or those struggling with opioid withdrawal and depressive symptoms.
For these reasons, the decision to start or continue taking Contrave while on Haldol should be made in consultation with a trusted doctor or pharmacist, ideally one who understands how the combination could affect the patient’s metabolism, drug effects, and risk of side effects.
Why Interactions Matter: Contrave’s Bupropion Component
The primary concern when combining Haldol with Contrave lies in the bupropion treatment. Bupropion is a known seizure threshold-lowering agent. Its presence in Wellbutrin SR, Wellbutrin XL, and Contrave extended-release tablets is associated with an increased risk of seizures—particularly in those with preexisting seizure disorder or who have suddenly stopped drinking alcohol.
“The combination of bupropion and haloperidol may amplify the risk of neurological side effects. Patients with any risk factors for seizures or psychiatric instability need to be evaluated very carefully,” says Dr. Matthew Olesiak, Chief Medical Director at SANE MD.
The boxed warning alerts doctors about the suicidal thoughts and behaviors associated with antidepressants, including bupropion hydrochloride. While it can support weight loss, smoking cessation, and mental health, these benefits come with an extensive list of possible side effects.
Potential Side Effects When Combining Contrave and Haldol
Combining Contrave and Haldol introduces a significant concern for overlapping and potentially amplified side effects, particularly those involving the nervous system, cardiovascular function, and mental health. The interaction between these two medications is not merely additive—it may produce unpredictable effects that require careful monitoring by a healthcare provider.
While each drug has its own profile of adverse reactions, using them together can increase the burden on the brain, liver, and cardiovascular system.
The most commonly reported side effects in patients combining these drugs include:
- Tremors: Involuntary shaking or trembling, especially in the hands or arms, may occur due to dopamine receptor interference from Haldol, which is further aggravated by bupropion’s effect on neurotransmitter levels.
- Restlessness or agitation: Known as akathisia, this inner sense of unease or inability to stay still is frequently associated with antipsychotics like Haldol and may be intensified by the stimulant-like properties of bupropion in Contrave treatment.
- Muscle stiffness: Also called rigidity, this symptom reflects abnormal muscle tone and is a hallmark of extrapyramidal symptoms (EPS). It can impair mobility and quality of life.
- Cognitive dulling or confusion: These symptoms result from disrupted neurotransmitter activity and may be worsened by increased systemic exposure to haloperidol when combined with bupropion.
- Suicidal thoughts and behaviors: Both bupropion hydrochloride and Haldol carry boxed warning risks for inducing or worsening suicidal thoughts and behaviors, especially in younger adults or those with untreated bipolar disorder.
- Dizziness or fainting: These may stem from blood pressure fluctuations, medication-induced sedation, or neurologic side effects—a risk heightened when taking Contrave with other CNS-active drugs.
- Low blood sugar: Though uncommon, low blood sugar can result from medication-related appetite suppression, altered eating patterns, or interactions with other drugs used for diabetes or metabolic disorders.
- High blood pressure: Both Contrave and Haldol have been independently associated with elevated blood pressure. When taken together, they can increase the risk of high blood pressure—a serious concern for individuals with cardiovascular risk factors or pre-existing hypertension.
Extrapyramidal Symptoms (EPS)
Both medications are capable of triggering extrapyramidal symptoms, which are drug-induced movement disorders.
These can present as:
- Involuntary facial grimacing
- Lip smacking or tongue movements
- Parkinsonian tremors
- Muscle rigidity
- Restlessness or pacing
While EPS is more commonly associated with antipsychotics like Haldol, taking Contrave—especially in patients sensitive to bupropion treatment—can compound the problem. This happens because bupropion hydrochloride affects dopamine levels, possibly interfering with haloperidol’s action in the brain’s basal ganglia, where movement is regulated.
Metabolic Concerns: Bupropion’s Impact on Haldol Levels
One lesser-known risk is that bupropion hydrochloride is a known inhibitor of the enzyme CYP2D6, which is involved in the metabolism of many prescription drugs, including Haldol. By inhibiting this enzyme, bupropion treatment can reduce the rate at which haloperidol is broken down, increasing its concentration in the bloodstream. This can result in increased risk of side effects, including sedation, movement disorders, and mental health changes like paranoia or emotional blunting.
This altered metabolism, referred to as increased systemic exposure, is especially important for older adults or those with impaired liver function, as it further complicates drug clearance and dosage adjustment decisions.
Psychiatric and Behavioral Side Effects
Behavioral and psychiatric side effects can also be severe. Some patients report:
- Worsening depression
- Irritability or aggression
- Anxiety or panic attacks
- Mania or hypomania (particularly in those with undiagnosed bipolar disorder)
- Emotional detachment or “flat affect”
The FDA boxed warning alerts doctors to the potential for suicidal thoughts and behaviors with any antidepressant drugs, including both bupropion and naltrexone combinations. Haldol also carries risks for mental health instability, especially when used at higher doses or in combination with other medications that act on the central nervous system.
Because of this, patients should be routinely screened for mental health deterioration during Contrave treatment, especially if they’re already taking Haldol or being evaluated for bipolar disorder, schizophrenia, or major depressive disorder.

Seizure Risk and the Lowered Seizure Threshold
Taking Contrave poses a well-documented risk of seizures, especially at higher doses or in patients with a seizure disorder. Haldol, while not a known seizure-inducer on its own, can also lower the seizure threshold in sensitive individuals.
This combination may be dangerous for:
- Those with epilepsy or a seizure disorder
- Patients with bipolar disorder
- People undergoing opioid withdrawal
- Individuals with severe hepatic impairment
- Those who have suddenly stopped drinking alcohol
“Even in people without a known history of epilepsy, combining medications that lower the seizure threshold is risky,” adds Dr. Olesiak. “Anyone starting Contrave treatment should disclose all medications, even over the counter drugs.”
If you have experienced a seizure before or have other risk factors—including head trauma or an eating disorder—this combination may significantly increase the risk of future events.
Blood Pressure Concerns
Blood pressure elevation is another shared side effect of both medications. According to a study published in the American Journal of Clinical Pharmacology, treatment with Contrave (naltrexone/bupropion) has been associated with modest increases in systolic blood pressure, particularly during the initial weeks of therapy or after dose adjustments. In contrast, Haldol (haloperidol) may cause orthostatic hypotension or, in some patients, elevated blood pressure, depending on individual response.
Healthcare providers must monitor blood pressure regularly in patients taking Contrave, especially if they are also prescribed Haldol or other medications that affect cardiovascular function.
Mental Health and Behavioral Concerns
Both Haldol and bupropion treatment can cause mental health changes—ranging from mood swings and suicidal thoughts and behaviors to hallucinations. These side effects are more likely in those with underlying bipolar disorder or major depressive disorder. In rare cases, serotonin syndrome occurs, particularly when other drugs affect the serotonergic neurotransmitter system.
Patients with these conditions must be closely monitored during treatment. The boxed warning for antidepressant drugs emphasizes that mood disorders may worsen or lead to suicidal thoughts and behaviors in vulnerable individuals.
If you or a loved one experiences sudden mood changes, hallucinations, or dangerous behavior patterns while taking Contrave, seek help immediately. Call your local emergency number or the suicide and crisis lifeline.
What Increases the Risk of Side Effects?
Certain risk factors amplify the likelihood of adverse outcomes when combining these drugs. These include:
- History of mental health conditions
- Concurrent use of systemic corticosteroids
- Use of prescription drugs that lower the seizure threshold
- Use of other weight loss drugs
- Lack of dose reduction or dosage adjustment
- Use of over-the-counter stimulants or herbal products like St. John’s Wort
Discuss any medical conditions, including past mental illness, seizures, or liver issues, with your doctor or pharmacist before starting Contrave.
Special Populations: Who Should Be Extra Cautious?
Older Adults
Seniors are more sensitive to side effects like confusion, dizziness, and low blood sugar. The combination of Contrave and Haldol should be considered carefully in this group.
Teens and Young Adults
There is a known increased risk of suicidal thoughts and behaviors in this age group when using antidepressant drugs such as bupropion hydrochloride.
People Undergoing Opioid Detox
Contrave contains drugs called opioid antagonists like naltrexone hydrochloride, which can worsen opioid withdrawal symptoms if taken too soon after the last opioid use. Combining Haldol may further complicate these adverse reactions.
How to Minimize Risk When Taking Contrave and Haldol
- Always disclose other medications and over-the-counter drugs.
- Avoid high-fat meals, which increase absorption and the risk of side effects during Contrave treatment.
- Consider a dose reduction if you’re experiencing strong side effects.
- Follow a structured, reduced-calorie diet to optimize weight loss without over-relying on medication.
- Schedule regular mental health and blood pressure check-ins with your provider.
When to Call for Help
Seek urgent care or dial your local emergency number if you experience:
- Seizures
- Chest pain or irregular heartbeat
- Hallucinations or delusional thoughts
- Difficulty breathing or a severe allergic reaction
- Intense suicidal thoughts
These may signal a medical emergency and require immediate attention.
Can You Still Use Both?
In some cases, healthcare professionals may choose to prescribe Contrave and Haldol together—especially when there are no better alternatives. This will depend on your health history, body weight, initial body mass index, and how well you’ve tolerated other drugs in the past.
However, this approach requires ongoing monitoring, frequent assessments, and full transparency with your doctor or pharmacist.
Frequently Asked Questions (FAQ)
When it comes to taking Contrave—especially alongside medications like Haldol—it’s natural to have questions about safety, effectiveness, and potential drug interactions.
Below are answers to some of the most common questions patients ask about Contrave treatment, bupropion hydrochloride, and managing side effects while achieving successful weight loss outcomes.
1. What medications should I avoid with Contrave?
Contrave drug interactions are prevalent with many different medications. Patients should avoid combining Contrave with any MAOI medications like Zyvox, drugs that lower the seizure threshold, such as other antidepressant drugs (Zoloft), antipsychotics, NSAIDs, stimulants (Ritalin), epilepsy medications like Tegretol, or over-the-counter cold medicines like Benadryl containing decongestants. Even Tylenol can interact negatively with Contrave.
Additionally, opioid medications like morphine and codeine, including opiate agonists, must be avoided due to the naltrexone hydrochloride component, which can trigger acute opioid withdrawal symptoms. Using other weight loss drugs like Qsymia at the same time may also increase the risk of dangerous side effects.
Always tell your doctor or pharmacist about every medication, supplement, or herbal product you’re taking before starting Contrave treatment.
2. Does bupropion interact with haloperidol?
Yes, bupropion hydrochloride, found in both Contrave and Wellbutrin SR, can interact with haloperidol (Haldol) in ways that affect drug metabolism and increase the potential for side effects. Bupropion inhibits the liver enzyme CYP2D6, which plays a role in breaking down Haldol. As a result, Haldol may build up in the bloodstream, leading to greater systemic exposure and increased risk of movement disorders, sedation, and behavioral changes.
These Contrave interactions are particularly concerning for individuals with mental health conditions or a history of seizure disorders.
3. Can you take Contrave if you have bipolar disorder?
Caution is strongly advised when prescribing Contrave to individuals with bipolar disorder, especially if the condition is not well-controlled. The bupropion hydrochloride component may trigger manic or hypomanic episodes, and the risk of mental health changes, including suicidal thoughts and behaviors, is elevated. Healthcare providers may consider dose reduction, frequent monitoring, or alternative therapies depending on the severity of the disorder and other medical conditions.
It’s essential to have an in-depth conversation with your doctor or pharmacist before starting Contrave treatment if you have any history of bipolar disorder or major depressive disorder.
4. How to maximize weight loss on Contrave?
To support effective weight loss while taking Contrave, it’s important to follow a structured plan that includes a reduced-calorie diet, regular physical activity, and close communication with your healthcare team. Avoiding high-fat meals is crucial, as they can increase the absorption of Contrave extended release tablets and heighten the risk of side effects.
Patients should also be consistent with their dosage schedule and avoid missing doses to maintain steady blood levels of the medication. Setting realistic goals and addressing emotional eating or underlying mental health concerns can further enhance success with Contrave treatment.
5. What medications should not be taken with Contrave?
Certain prescription drugs and over-the-counter drugs should not be combined with Contrave due to the potential for harmful Contrave interactions. These include other medications that increase seizure risk, such as tramadol, antipsychotics like Haldol, stimulants like Adderal or systemic corticosteroids. Patients taking opioids or drugs for opioid withdrawal must avoid Contrave, as naltrexone hydrochloride can lead to severe adverse reactions.
If you have a history of seizures, liver problems, or suddenly stopped drinking alcohol, you must notify your provider before taking Contrave, as these factors significantly increase the risk of dangerous outcomes.
6. Can you take Haldol with Wellbutrin?
Combining Haldol with Wellbutrin SR or Wellbutrin XL (both containing bupropion hydrochloride) is generally not recommended without close medical supervision. The combination may increase the risk of neurological side effects, such as tremors, stiffness, or extrapyramidal symptoms, and can further lower the seizure threshold. Bupropion’s interference with liver enzymes may also elevate Haldol levels, leading to adverse reactions like sedation or worsening mental health changes.
If both medications are necessary, your doctor may adjust the doses or monitor for complications, especially in patients with medical conditions like a seizure disorder or bipolar disorder.
Final Thoughts
The combination of Contrave and Haldol is not inherently unsafe but does come with significant risks, particularly relating to the seizure threshold, mental health, and blood pressure regulation. Patients should weigh the benefits of weight loss and symptom control against the increased risk of serious side effects.
If you’re considering this combination or are already taking Contrave, be honest with your healthcare provider about your current medications, medical conditions, and treatment goals.
References
American Journal of Clinical Pharmacology