Contrave and Xanax Drug Interactions: What You Need to Know

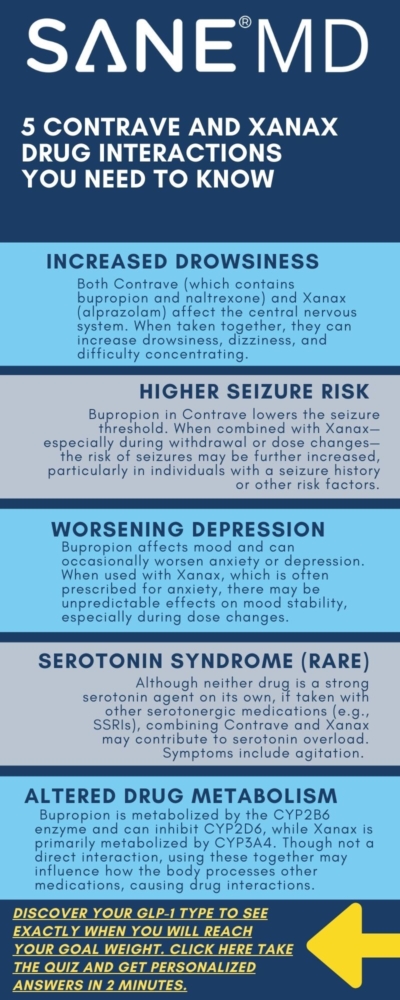
When you’re taking multiple medications like Contrave and Xanax, understanding potential drug interactions is critical. Contrave is a prescription medication used to support weight loss in certain individuals, while Xanax (alprazolam) is often prescribed for anxiety and panic disorders. Together, these drugs can cause overlapping effects that may increase the risk of side effects or trigger new health complications.
Although both are effective within their own therapeutic categories, combining them requires a clear understanding of their mechanisms and the ways they may interact in the body. If you’re taking Contrave or considering this drug combination, being informed about Contrave and Xanax drug interactions can help you make safer decisions about your treatment plan.
Key Takeaways
- Combining Contrave and Xanax may increase the risk of side effects such as dizziness, drowsiness, confusion, and difficulty concentrating.
- Patients with certain medical conditions, especially uncontrolled high blood pressure or seizure disorders, should talk with their doctor before taking Contrave.
- Always tell your doctor about other drugs, supplements, or over-the-counter products you’re using to prevent interactions.
What Is Contrave?
Contrave is a combination medication containing naltrexone and bupropion, both of which are used in extended-release oral tablets. It is one of several prescription weight loss drugs approved to help reduce appetite and control cravings, especially when combined with diet and exercise.
Contrave works through multiple pathways in the brain to decrease appetite, making it helpful for certain individuals struggling with obesity or weight-related health issues like high blood pressure or low blood sugar.
However, Contrave drug interactions are common, potentially causing adverse effects, including increased risk of seizures, suicidal thoughts, and mental health changes, especially in those with bipolar disorder or a seizure disorder.
What Is Xanax?
Xanax is part of a class of medications called benzodiazepines. It’s primarily used to treat anxiety disorders and sometimes prescribed short-term for panic attacks. It acts quickly to calm the nervous system but can lead to physical dependence with prolonged use.
Because Xanax affects the central nervous system (CNS), mixing it with other medications that also act on the brain can increase sedation or slow down vital functions like breathing or heart rate.
Contrave and Xanax Drug Interactions Summary Table
| Category | Key Information |
|---|---|
| Drug Names | Contrave (bupropion + naltrexone) and Xanax (alprazolam) |
| Primary Uses | Contrave: weight loss support; Xanax: anxiety and panic disorders |
| Main Interaction Risks | Sedation, confusion, seizures, impaired breathing, worsening mental health symptoms |
| High-Risk Conditions | Seizure disorder, bipolar disorder, uncontrolled high blood pressure, liver problems, history of suicidal thoughts |
| Avoid With | Alcohol, grapefruit juice, MAOIs, other CNS depressants, bupropion-containing drugs, certain antibiotics |
| Emergency Symptoms | Extreme drowsiness, slowed breathing, seizures, allergic reaction, persistent dark urine, suicidal thoughts |
| Monitoring Needed | Blood pressure, mood changes, signs of CNS depression, seizure activity |
| Patient Safety Tips | Tell your doctor all medications you’re taking, including OTC and supplements; follow provided medication guide and patient package insert |
| FAQ Highlights | Combining benzos with Contrave requires caution; naltrexone doesn’t block Xanax but may alter its effects; drug list review is essential to prevent interactions |
Contrave and Xanax: Understanding the Drug Combination
Although Contrave and Xanax are used for different purposes—weight loss vs. anxiety—there’s a possibility that using them together could lead to certain drug interactions. Both medications impact neurotransmitters in the brain and can affect mental clarity, energy, and alertness.
“Both naltrexone and bupropion influence brain chemistry, and when combined with a sedative like Xanax, there’s a heightened potential for CNS-related side effects,” says Dr. Matthew Olesiak, Chief Medical Director at SANE MD.
Some people taking Contrave experience insomnia or agitation due to its bupropion component. If Xanax is used to counteract these effects, it may mask early signs of mental health conditions or drug-related complications. This can be especially dangerous for patients with a history of bipolar disorder, suicidal thoughts, or other mental health conditions.
Furthermore, starting Contrave treatment while already using Xanax—or vice versa—requires careful dose adjustment and supervision by a healthcare provider.
Risks and Side Effects to Watch For
The risk of side effects from combining Contrave and Xanax may vary based on your dosage, age, underlying medical conditions, and overall health history. People with mental health conditions, a history of seizure disorder, or those taking other drugs that act on the central nervous system should be especially cautious.
This drug combination can trigger a range of possible interactions, such as:
- Drowsiness or sedation: Xanax is a sedative, and bupropion in Contrave can increase alertness in some but cause fatigue in others. The mixture may lead to overwhelming tiredness, especially when starting Contrave treatment.
- Dizziness and confusion: These symptoms may impair your ability to drive, work, or carry out daily tasks safely—especially if you also drink alcohol or consume grapefruit juice, which can intensify these effects.
- Slowed breathing: Central nervous system depression is a serious concern when mixing drugs like Xanax with medications that can alter neurological function.
- Difficulty concentrating: People taking Contrave and Xanax together may experience reduced mental sharpness or “brain fog,” particularly in the first few weeks of combined use.
- Risk of seizure: Bupropion carries a dose-dependent increased risk of seizures, particularly in those with eating disorders, prior head trauma, or concurrent use of other stimulants or sedatives. Combining it with CNS depressants like Xanax further complicates this risk, especially in patients with a known seizure disorder.
Additionally, both medications can contribute to mental health changes. Bupropion—used in Contrave—is classified as an atypical antidepressant and can treat depression, but it may also cause agitation, insomnia, or suicidal thoughts, particularly in adolescents and young adults. The boxed warning alerts doctors to this possibility and urges careful monitoring during the initiation of therapy.
“Because of the psychological components of both medications, patients should be closely monitored when combining Contrave and Xanax, particularly during the first few weeks of therapy,” adds Dr. Olesiak.
Increased risk of sedation may also heighten the potential for injuries, especially in older adults, who are more sensitive to changes in drug metabolism. Falls, head trauma, and related complications are more likely when cognitive or motor skills are impaired.
Moreover, the risk of side effects may be compounded if patients are taking other forms of benzodiazepines, certain sleep aids, or over-the-counter antihistamines. These other medications can further suppress CNS activity, creating a dangerous drug synergy.
People with uncontrolled high blood pressure may also face a worsening of symptoms. Contrave can increase blood pressure and heart rate, while sedatives like Xanax may mask warning signs until the condition becomes more serious.
Signs of a possible allergic reaction—such as rash, itching, swelling, or dark urine—should be reported immediately. These could indicate liver strain, especially in people with pre-existing liver problems or those who drink alcohol frequently.
Lastly, those who suddenly stop drinking alcohol or rapidly discontinue Xanax may experience withdrawal symptoms, including mood swings, tremors, or seizures. This makes it essential to talk with your doctor before making any changes to your treatment regimen.
Alcohol, Grapefruit Juice, and Other Interactions
If you’re taking Contrave, it’s important to avoid drinking alcohol or suddenly stop drinking alcohol, as both can amplify the drug’s effects on the nervous system and liver. Drinking while on Xanax can also dangerously depress breathing or increase the risk of blackouts. Similarly, taking an opioid withdrawal drug, such as Suboxone with Contrave, can negatively impact the central nervous system, potentially leading to dangerous symptoms.
Grapefruit juice is another concern. It can interfere with the enzymes that process many medications, including Xanax and bupropion, leading to increased drug effects or risk of side effects. This interaction may not be obvious, which is why it’s critical to talk with your doctor before making any changes to your diet or medications.
Who Should Be Extra Cautious?
You should talk with your doctor if you:
- Have uncontrolled high blood pressure or severely high blood pressure. Check out our article “Does Contrave Increase Blood Pressure” to learn more.
- Have a seizure disorder or liver problems
- Are pregnant or breastfeeding (breast milk can pass certain ingredients)
- Have a history of mental health or mood disorders
- Are using macrolide antibiotics or over-the-counter cold or allergy products
People with health conditions such as diabetes should also be cautious due to the potential for low blood sugar when starting Contrave treatment. Always disclose all medications, supplements, and even lab tests you’re undergoing to help prevent interactions.

How to Use Contrave and Xanax Safely
Whether you’re already taking Contrave or considering combining it with Xanax, your first step should always be open communication with a trusted healthcare provider. The most important thing you can do is tell your doctor about everything you’re taking—including prescription medications, over-the-counter supplements, herbal remedies, and vitamins. Even vitamin interactions or seemingly mild other drugs may have an impact on how your body processes either Contrave or Xanax.
Make sure to also disclose any current or past medical conditions, such as:
- Heart disease
- Respiratory issues
- Spinal cord injuries
- Mental health conditions or episodes (e.g., depression, anxiety, bipolar disorder)
- History of seizure disorder
- Liver problems or kidney impairment
- History of drug or alcohol use
Being honest about your full health history helps your healthcare professional identify possible interactions and guide you safely through Contrave treatment. It also reduces your risk of side effects, especially when adding Xanax or other medications to your routine.
Here’s how your provider can help manage this drug combination safely:
- ✅ Evaluate your full health history to detect potential risks or health factors that could make interactions more dangerous.
- ✅ Adjust doses or recommend other treatments if the combination of Contrave and Xanax is too risky for your current condition.
- ✅ Monitor for withdrawal symptoms, behavioral shifts, or early signs of complications—particularly if you experience mental health changes or suicidal thoughts.
- ✅ Offer a clear medication guide or patient package insert to ensure you understand potential adverse effects, signs of a serious warning, and how to prevent interactions.
“Medication safety starts with transparency. Sharing every supplement, prescription, and past condition—even if it feels minor—gives your provider the full picture needed to manage drug interactions effectively,” says Dr. Matthew Olesiak, Chief Medical Director at SANE MD.
Before you start Contrave treatment, review all the drug information contained in the manufacturer’s labeling and discuss it with your pharmacist or physician. This includes warnings about grapefruit juice, drinking alcohol, withdrawal symptoms, and monitoring for signs of low blood sugar, dark urine, or a developing allergic reaction.
In some cases, lab tests may be required to monitor your blood pressure, liver enzymes, or kidney function during ongoing treatment. This is especially true if you’re taking extended-release oral tablets, have other mental health diagnoses, or are on long-term therapy with other forms of medication.
Lastly, always have a plan in place in case of an emergency. If you experience sudden chest pain, confusion, shortness of breath, or signs of overdose, call your local emergency number immediately. Keeping an updated list of your medications on hand—and sharing it with any doctor or specialist you see—can prevent errors and save time during urgent care situations.
Signs of a Medical Emergency
While Contrave and Xanax drug interactions may not cause problems in everyone, they can trigger potentially life-threatening reactions in certain individuals. Knowing when to act quickly is crucial—especially during the first few weeks of starting Contrave treatment, when your body is still adjusting to new medications.
If you experience any of the following symptoms after combining these drugs, call your local emergency number or go to the nearest emergency room without delay:
- Extreme drowsiness or confusion: This may signal excessive CNS depression from combining two drugs that affect brain activity. It may also impair your ability to communicate, react, or breathe properly.
- Irregular or slowed breathing: This is a red flag for respiratory depression—a rare but dangerous side effect when sedatives like Xanax are combined with other medications that influence the central nervous system.
- Seizure: If you have a known seizure disorder, your risk of side effects increases significantly when taking Contrave. Seizures can occur suddenly and without warning, requiring immediate medical attention.
- Sudden allergic reaction: Watch for hives, itching, swelling (especially of the face or throat), and shortness of breath. A severe allergic reaction can escalate into anaphylaxis, a life-threatening condition that requires urgent care.
- Persistent dark urine: This may indicate liver problems or a serious warning sign of internal organ distress. It’s especially important to report this if you also experience yellowing of the skin or eyes (jaundice), abdominal pain, or nausea.
- Signs of low blood sugar: These include shakiness, sweating, dizziness, and confusion. People with diabetes who are taking Contrave may experience low blood sugar, especially if doses of insulin or other antidiabetic drugs aren’t adjusted properly.
- Worsening suicidal thoughts: Contrave contains bupropion, which has been linked to changes in mood, agitation, and thoughts of self-harm. If these symptoms intensify, contact a healthcare provider or emergency services immediately.
Other symptoms that may signal a medical emergency include severe headaches, chest pain, fainting, hallucinations, or unresponsiveness. These events may indicate adverse effects tied to possible interactions with other drugs, or underlying health conditions exacerbated by the drug combination.
Never ignore a serious warning from your pharmacist, doctor, or the official medication guide regarding potential drug reactions. Follow-up is especially critical when combining medications that affect your mental state, metabolism, or nervous system.
If you’re ever unsure whether a symptom is cause for concern, it’s better to err on the side of caution—talk with your doctor, contact your healthcare provider, or call your local emergency number to be safe.
Frequently Asked Questions (FAQ)
Combining medications like Contrave, Xanax, and other central nervous system drugs can be confusing and risky without the right guidance.
Below are some of the most common questions patients ask about Contrave interactions, including how it works with benzodiazepines, bupropion, and naltrexone. Always consult a healthcare provider before making any changes to your medication regimen.
1. Can you take benzos with Contrave?
Benzodiazepines (like Xanax, Ativan, or Valium) can sometimes be taken with Contrave, but doing so carries an increased risk of side effects such as drowsiness, dizziness, slowed reflexes, and cognitive impairment. Both types of medications affect the brain, though in different ways—Contrave stimulates activity through bupropion and naltrexone, while benzos suppress it. This can create a neurological imbalance or mask signs of mental health changes.
If you’re taking Contrave and need a benzodiazepine, your healthcare provider may need to adjust dosages or monitor your response closely. It’s essential to tell your doctor about all the drugs you’re using to reduce your risk of dangerous drug interactions.
2. Can I take Xanax and Bupropion together?
Xanax and bupropion (one of the two active ingredients in Contrave) can be used together in some cases, but caution is necessary. Bupropion can lower the seizure threshold, and combining it with CNS depressants like Xanax may increase the likelihood of seizures, sedation, or mood-related side effects. Patients with a history of bipolar disorder, mental health conditions, or substance use disorders are especially vulnerable to adverse effects when using both medications.
Always consult a healthcare provider to assess your individual health history and avoid possible interactions. Dose timing and frequency may need to be adjusted to ensure safety.
3. What medications should not be taken with Contrave?
Several medications should be avoided when taking Contrave, including monoamine oxidase inhibitors (MAOIs), certain antipsychotics, opioids like morphine, codeine, methadone, and fentanyl, macrolide antibiotics, and other drugs that lower the seizure threshold. Combining Contrave with other bupropion-containing products or medications that affect blood pressure or mental health may also pose a risk.
Additionally, drugs used to manage seizure disorders, uncontrolled high blood pressure, or conditions involving liver problems may worsen Contrave’s side effects. Grapefruit juice, alcohol, and some over-the-counter stimulants can also affect how Contrave works in your body. Always provide your full medication list to your healthcare provider to help prevent interactions.
4. What happens if you take Xanax on naltrexone?
Naltrexone, one of the components of Contrave, is an opioid antagonist, meaning it blocks the effects of opioids. While it doesn’t directly block benzodiazepines like Xanax, taking both together can still affect the central nervous system. This combination may dull or alter Xanax’s sedative effects and can make drug effects less predictable. It may also increase the risk of suicidal thoughts, confusion, or emotional instability, especially in people with coexisting mental health conditions.
Always talk with your doctor before combining naltrexone and Xanax, particularly if you are in recovery from substance use or being treated for anxiety.
Final Thoughts
Combining Contrave and Xanax isn’t always dangerous, but it does require thoughtful planning and supervision from a healthcare provider. With a growing number of people using weight loss drugs, understanding Contrave interactions has never been more important.
Always talk with your doctor before beginning, stopping, or adjusting medications. Knowing your personal health factors and following proper guidance can reduce your risk of side effects and help you stay safe while getting the treatment you need.
If you’re unsure, ask your healthcare professional for a medication guide or to go over your list of other drugs, including potential vitamin interactions and other interactions that could cause complications.

Modafinil and Contrave Drug Interactions: Safety Guide

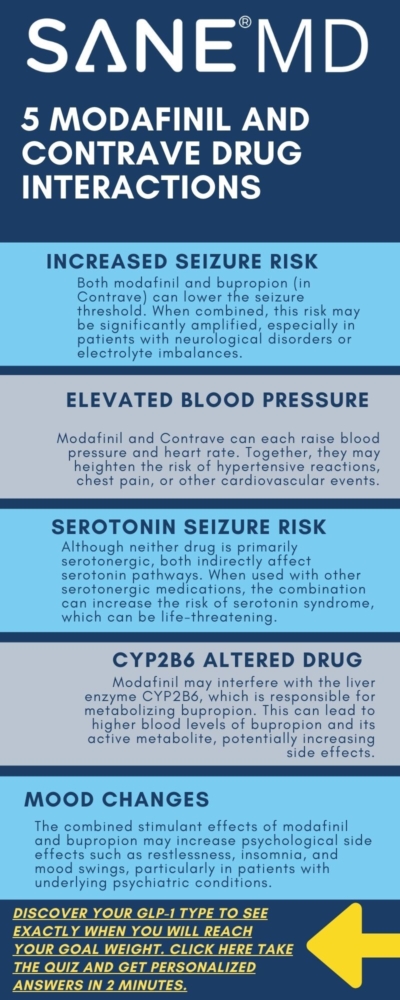
As more patients seek comprehensive approaches to improve focus, manage weight, and combat fatigue, the combination of medications like Contrave and modafinil is becoming increasingly common. However, this trend raises important safety concerns. The interaction between these two medications is not widely studied in clinical trials, making careful consideration and medical guidance essential for anyone considering or currently using both.
This guide examines the known and potential modafinil and Contrave drug interactions, highlights the increased risk of side effects, and provides guidance on monitoring, dosage adjustment, and risk factors.
Key Takeaways
- Combining Contrave and modafinil may increase the risk of seizures, serotonin syndrome, and elevated blood pressure. Monitoring is critical for patients on both medications.
- Contrave contains bupropion and naltrexone—two active compounds with unique effects on the brain’s reward system, which may intensify adverse reactions when combined with modafinil.
- Physicians must weigh the therapeutic benefits of this combination against potential complications, especially for patients with a history of psychiatric disorders, substance use, or cardiovascular conditions.
Understanding Contrave and Modafinil
Contrave is a fixed-dose combination medication composed of two active ingredients: bupropion and naltrexone. Together, they offer a unique dual mechanism of action aimed at addressing the neurochemical drivers behind overeating and cravings. Approved by the FDA for chronic weight management, Contrave is prescribed for certain adults with an initial body mass index (BMI) of 30 or higher, or 27 and above if the patient also has a weight-related condition such as diabetes mellitus, high cholesterol, or hypertension.
The first component, bupropion, is an atypical antidepressant most commonly used in treating major depressive disorder and smoking cessation. It works by inhibiting the reuptake of dopamine and norepinephrine—key neurotransmitters in the brain’s reward system. Through this action, bupropion can reduce the psychological urge to eat for comfort or reward.
The second ingredient, naltrexone hydrochloride, is an opioid receptor antagonist typically used to treat alcohol and opioid addiction. By blocking opioid receptors in the brain, naltrexone dampens the pleasure response associated with certain behaviors—like eating highly palatable foods. This makes it easier for compatible patients to resist cravings, particularly during the early phase of a reduced-calorie diet.
Together, bupropion naltrexone produces therapeutic effects that extend beyond simple appetite suppression. The combination aims to rebalance disrupted brain signaling related to reward and self-control, allowing for more sustainable weight loss among certain obese adults or those with weight-related comorbidities.
Modafinil, in contrast, is a wakefulness-promoting agent. It is FDA-approved for the treatment of excessive daytime sleepiness associated with narcolepsy, shift work sleep disorder, and obstructive sleep apnea. Unlike traditional stimulants, modafinil does not have a direct amphetamine-like mechanism. Instead, it enhances dopaminergic effects by inhibiting the dopamine transporter receptor, resulting in increased extracellular dopamine levels in key areas of the brain that govern alertness and attention.
Although not approved for this purpose, modafinil is sometimes used off-label to assist with weight loss due to its energy-boosting and appetite-suppressing effects. Some individuals report that it reduces the urge to snack or overeat, especially when combined with calorie restriction. However, this off-label use carries potential safety concerns—particularly when modafinil is used alongside medications that already affect the central nervous system, such as Contrave.
Both drugs target overlapping neural circuits, which is part of what raises red flags about modafinil and contrave drug interactions. Since they can influence reward, motivation, energy, and mood, their combined use may lead to amplified effects—or unintended complications.
Modafinil and Contrave Drug Interaction Summary
Combination Overview, Risks, and Monitoring Considerations
| Category | Details |
|---|---|
| Drugs Involved | Modafinil and Contrave (bupropion/naltrexone) |
| Primary Concerns | Increased risk of seizures, elevated blood pressure, serotonin syndrome, and mood instability |
| CNS Impact | Both modafinil and bupropion influence dopamine and norepinephrine; overlapping mechanisms may amplify stimulation and lower seizure threshold |
| Serotonin Syndrome Risk | Potential risk when combined with serotonergic agents; modafinil and bupropion may contribute indirectly |
| Cardiovascular Risks | May cause hypertension, chest pain, and cardiac strain—especially in patients with obesity, heart disease, or high blood pressure |
| Mental Health Concerns | May increase agitation, insomnia, anxiety, or mood swings; greater risk in patients with bipolar disorder, OCD, or history of suicidal ideation |
| Drug Metabolism Interaction | Modafinil affects CYP2B6, possibly altering bupropion and hydroxybupropion levels; may raise blood concentration and side effect risks |
| Contraindicated Medications | Opiate agonists (e.g., codeine, morphine), monoamine oxidase inhibitors (MAOIs) |
| Caution With | Tricyclic antidepressants, SSRIs, SNRIs, systemic corticosteroids, hormonal contraceptives |
| Common Side Effects (Combined) | Headache, nausea, abdominal pain, joint pain, insomnia, restlessness/anxiety |
| Serious Adverse Reactions | Seizures, hypertensive crisis, serotonin syndrome, manic episodes, chest pain |
| Monitoring Recommendations | Monitor blood pressure, mood changes, and signs of serotonin syndrome or seizure activity; regular check-ins advised |
| Dosing Guidelines | Gradual titration recommended; avoid high-fat meals with Contrave; dose adjustments may be necessary |
| Patient History Warnings | Assess for opioid use, alcohol dependence, psychiatric conditions, and use of other serotonergic or CNS-acting drugs |
| Off-Label Use Considerations | Modafinil may be used off-label for weight loss and attention; increased interaction risk if also used for smoking cessation or with additional CNS-active medications |
| Doctor Quote | “Combining stimulant-like medications can elevate the risk of seizures and increased blood pressure, particularly in individuals with underlying psychiatric disorders or cardiovascular issues.” – Dr. Matthew Olesiak, MD |
Why Combining These Medications Raises Concerns
While there is only limited data on modafinil and Contrave drug interactions, their shared impact on the central nervous system warrants caution. Both bupropion and modafinil influence neurotransmitters like dopamine and norepinephrine, potentially increasing stimulation beyond a safe threshold.
According to Dr. Matthew Olesiak, Chief Medical Director at SANE MD,
“Combining stimulant-like medications can elevate the risk of seizures and increased blood pressure, particularly in individuals with underlying psychiatric disorders or cardiovascular issues.”
Additionally, bupropion inhibits the reuptake of dopamine and norepinephrine, and modafinil further enhances dopaminergic activity. This overlapping effect can raise systemic exposure and heighten the chance of serotonin syndrome, particularly when combined with other drugs affecting the serotonergic neurotransmitter system.
Increased Risk of Seizures
Among the most serious risks of combining these medications is the seizure threshold being lowered. Patients receiving bupropion, especially those with preexisting neurological conditions or electrolyte imbalances, are at higher risk. Modafinil may further compromise this threshold.
“Modafinil’s stimulation of the brain’s dopamine system may synergize with bupropion therapy in a way that reduces the seizure threshold significantly,” says Dr. Olesiak.
Cardiovascular Effects and Blood Pressure Monitoring
Both bupropion naltrexone and modafinil may cause increased blood pressure and chest pain, particularly in obese patients or those with congestive heart failure. Because Contrave can cause hypertensive reactions, and modafinil may also elevate blood pressure, patients must be monitored carefully for signs of cardiac strain. Sudden onset of joint pain, abdominal pain, or chest pain may occur and should be reported immediately.
A dosage adjustment or dose reduction may be needed if patients experience high blood pressure during treatment.
Impact on Mental Health
Patients with bipolar disorder, major depressive disorder, or obsessive-compulsive disorder should approach this combination with extreme caution. The stimulant effects of modafinil may exacerbate mood instability, while initiating bupropion therapy in such individuals has been associated with suicidal ideation and manic episodes.
Moreover, the combined use of these drugs may increase agitation, insomnia, and anxiety. These adverse reactions may occur in individuals without prior psychiatric diagnoses, especially if no dose adjustment is made over time.
Risk of Serotonin Syndrome
While serotonin syndrome is more commonly associated with the use of SSRIs, SNRIs, and monoamine oxidase inhibitors, it’s important to recognize that serotonin syndrome occurs when multiple medications—especially those that influence the serotonergic neurotransmitter system—lead to excess serotonin in the brain. This can happen even when the medications involved are not classified as traditional serotonergic drugs.
Both bupropion and modafinil have indirect effects on serotonin pathways. Bupropion inhibits the reuptake of norepinephrine and dopamine, and while it is not a primary serotonergic agent, it may still interact with other drugs that act on serotonin systems, raising the overall risk. Modafinil, though primarily known for its dopaminergic effects, has been shown to influence multiple neurotransmitters, including serotonin, especially when used alongside other drugs with serotonergic properties.
When these medications are combined—either with each other or with SSRIs, SNRIs, tricyclic antidepressants, or monoamine oxidase inhibitors—there is a theoretical and documented risk of serotonin syndrome, as demonstrated in Science Direct. Symptoms may include agitation, confusion, rapid heart rate, high blood pressure, tremor, muscle rigidity, and, in severe cases, seizures or respiratory depression. These reactions may occur rapidly and require immediate medical attention.
Because neither bupropion nor modafinil is traditionally flagged as a high-risk serotonergic agent, serotonin syndrome can be under-recognized in clinical settings. Healthcare providers should remain vigilant when prescribing these drugs in combination with other serotonergic agents or in patients with a history of psychiatric disorders, bipolar disorder, or obsessive-compulsive disorder, where polypharmacy is common.
Drug Interactions with Opiates, Alcohol, and Other Substances
Bupropion naltrexone is contraindicated with opiate agonists, such as morphine and codeine. Naltrexone, as an opioid antagonist, can precipitate opioid withdrawal symptoms, including respiratory depression, anxiety, and abdominal pain. This may occur even in individuals who are no longer actively using opioids but have residual dependency.
Opioid withdrawal or opioid addiction history must be ruled out before treatment initiation. This is especially important for patients being treated for alcohol and opioid addiction or undergoing nicotine replacement therapy, as bupropion inhibits the reward cycle reinforcement.
Likewise, alcohol dependence or active alcohol use may worsen adverse reactions, particularly joint pain, abdominal pain, and liver-related complications in those with severe hepatic impairment.

Common Side Effects and Adverse Reactions
When bupropion naltrexone and modafinil are taken together, the likelihood of experiencing adverse reactions increases due to their overlapping effects on the central nervous system and metabolism. While not everyone will experience problems, some symptoms are more commonly reported—especially during the early weeks of combined therapy or following a dosage adjustment.
The most frequently observed side effects in individuals using both medications include:
- Headache
- Nausea
- Abdominal pain
- Anxiety or restlessness
- Insomnia or disrupted sleep patterns
- Joint pain
These effects may occur independently or be amplified when the medications are used together. In many cases, they are mild and temporary—resolving as the body adapts to the medications. However, in some individuals, these reactions may occur persistently and require intervention. This could involve a dose reduction, a slower dosage increase, or even discontinuation of one of the drugs.
Importantly, some side effects—such as abdominal pain, joint pain, and chest pain—can mimic symptoms of more serious complications like cardiovascular events or hypertensive reactions. These should not be ignored and must be evaluated promptly by a healthcare provider.
In certain patients, side effects may emerge as part of broader psychiatric disorders, particularly if there’s a history of bipolar disorder, obsessive-compulsive disorder, or anxiety. These individuals may be more sensitive to changes in neurotransmitter levels caused by either drug.
At the biochemical level, the active metabolite of bupropion—known as hydroxybupropion—is largely responsible for the medication’s therapeutic and side-effect profiles. This metabolite is formed via the liver enzyme CYP2B6. However, modafinil is known to modulate cytochrome P450 activity, including CYP2B6, potentially interfering with the metabolic processing of bupropion, according to a study published on the NIH website.
This interference can lead to altered systemic exposure, resulting in statistically significant differences in the blood levels of bupropion and its metabolite. In real-world terms, this means that some patients may absorb too much of the active compounds, which could intensify side effects like high blood pressure, insomnia, or the risk of seizures.
Additionally, combining modafinil with other drugs that rely on the same metabolic enzymes—such as tricyclic antidepressants, antipsychotics, or systemic corticosteroids—could further complicate the body’s ability to safely process these substances. This increases the importance of reviewing all medications and supplements a patient is taking before starting combined therapy.
For those already on treatment, healthcare providers should monitor patients regularly for emerging symptoms and educate them on what to watch for—especially any signs of worsening abdominal pain, sustained anxiety, or chest pain. Early intervention can help prevent more serious complications and ensure the therapeutic effects of the treatment are not overshadowed by avoidable side effects.
Special Considerations for Dosing
Due to the increased risk of respiratory depression, abdominal pain, or seizure activity, gradual titration is essential. Physicians may recommend a slower dosage increase for Contrave when used with modafinil, especially in obese adults with body mass index thresholds above 30.
Also, taking Contrave with high-fat meals increases the rate of absorption, which may further complicate the interaction profile. A reduced-calorie diet is still recommended during contrave treatment, and patients should avoid fatty meals to minimize adverse reactions.
Smoking Cessation and Additional Therapeutic Use
Bupropion naltrexone is sometimes explored for smoking cessation, particularly for those with overlapping food cravings and nicotine dependence. Since modafinil also has off-label potential in attention and addiction disorders, the interaction profile may be complicated by therapeutic benefits across multiple domains, including neuropathic pain and attention-related issues.
Nevertheless, care must be taken not to assume enhanced efficacy simply because both medications affect mood, energy, or appetite. The combined therapeutic effects may be unpredictable and depend heavily on individual risk factors and metabolic rates.
Guidelines for Patients and Physicians
Patients considering or currently taking both Contrave and modafinil should:
- Disclose all current medications, including supplements and systemic corticosteroids or tricyclic antidepressants.
- Alert their doctor to any history of opioid addiction, alcohol dependence, or psychiatric disorders.
- Report side effects such as abdominal pain, joint pain, chest pain, or mood changes immediately.
- Understand that dose adjustment may be necessary at several stages of treatment.
- Avoid self-adjusting doses or substituting other drugs without physician oversight.
Frequently Asked Questions (FAQ)
Understanding how medications interact is essential for safety and treatment success.
Below are some of the most common questions about taking bupropion naltrexone (Contrave) and modafinil, as well as related drug combinations. Always consult your healthcare provider before starting or combining any medications.
1. Can you take modafinil and bupropion together?
Modafinil and bupropion may be taken together in some cases, but the combination should be approached with caution. Both drugs affect dopamine levels in the brain, which may increase the risk of seizures, especially in patients with a history of neurological conditions.
Additionally, modafinil may interfere with the metabolism of bupropion, potentially raising blood levels and the likelihood of adverse reactions. Doctors may recommend a dose adjustment or additional monitoring if these drugs are prescribed together.
2. What medications to avoid with Contrave?
Several medications should be avoided when taking Contrave due to potentially serious drug interactions. These include opiate agonists (such as codeine, hydrocodone, or morphine), as naltrexone may cause sudden opioid withdrawal symptoms. Monoamine oxidase inhibitors (MAOIs), used to treat depression, are also contraindicated, as combining them with bupropion therapy can lead to severe high blood pressure or serotonin syndrome. Other antidepressants can also cause adverse effects. Our recent article on taking Contrave and Paxil drug interactions explores this topic in depth.
Patients should also use caution with tricyclic antidepressants, antipsychotics, and other medications that lower the seizure threshold.
3. What drugs should not be taken with modafinil?
Medications that interact with the liver enzyme system—particularly CYP3A4 and CYP2B6—can be problematic when used with modafinil. This includes tricyclic antidepressants, hormonal contraceptives, and systemic corticosteroids, which may become less effective or increase the risk of side effects.
Additionally, modafinil can interfere with other drugs used to treat mental health conditions, increasing the risk of serotonin syndrome or cardiovascular effects. Patients with psychiatric disorders or those on complex regimens should be closely supervised if modafinil is introduced.
4. Can you take phentermine and Contrave at the same time?
Phentermine and Contrave are sometimes used together for weight loss, but this combination is not FDA-approved and carries certain risks. Both drugs can raise blood pressure and heart rate, increasing the chance of hypertensive reactions, chest pain, or abdominal pain in sensitive individuals.
There is also a concern about overstimulation of the central nervous system, which may heighten anxiety or the risk of seizures. If a physician considers combining them, they will likely recommend close monitoring and start with low doses to reduce potential harm.
Summary
Although combining modafinil and Contrave may seem appealing for patients aiming to lose weight while staying mentally alert, the combination introduces a web of possible drug interactions and side effects. The risk of seizures, increased blood pressure, serotonin syndrome, and opioid withdrawal symptoms makes it crucial for providers to monitor closely and educate patients thoroughly.
Physicians should review each patient’s history for opiate agonists, cardiovascular issues, and mental health conditions before initiating bupropion or adding modafinil. With tailored oversight, some patients may experience meaningful therapeutic effects, but safety must remain the top priority.
References

Taking Contrave and Nardil Together: Drug Interaction Guide

Combining prescription medications can be risky—especially when it involves drugs that affect brain chemistry. If you’re considering taking Contrave and Nardil together, it’s essential to understand how these medications might interact.
Both are powerful in their own right: Contrave is prescribed for weight loss for compatible individuals, while Nardil is a monoamine oxidase inhibitor (MAOI) used to treat depression. But taken together, they can increase the risk of side effects, including extremely high blood pressure, serious skin reactions, or even life-threatening events.
“Nardil is a very potent MAOI, and combining it with drugs like Contrave—particularly due to the bupropion component—can be dangerous without careful oversight,” explains Dr. Matthew Olesiak, Chief Medical Director at SANE MD. “This isn’t a casual combination—it requires clear justification and close monitoring by a qualified medical doctor.”
This guide breaks down the potential drug interactions, side effects to watch for, and why it’s crucial to talk with your doctor before combining these two medications.
Key Takeaways
- Combining Contrave and Nardil can cause serious or even life-threatening effects, including extremely high blood pressure, seizures, and allergic reaction symptoms.
- Contrave treatment is designed for certain individuals pursuing long-term weight management and should not be taken with MAOIs like Nardil without physician supervision.
- Always talk with your doctor about other medications you’re taking, especially if you’re being treated for mental disease, bipolar disorder, or eating disorders.
Understanding Contrave and Nardil
What Is Contrave?
Contrave is an FDA-approved prescription weight loss medication designed for long-term weight management in certain adults with a high body mass index (BMI), or those who are overweight with at least one weight-related condition like type 2 diabetes or high cholesterol.
It contains a combination of naltrexone and bupropion, two medications that affect different parts of the brain. Bupropion is a norepinephrine-dopamine reuptake inhibitor (NDRI) commonly used to treat depression and support smoking cessation, while naltrexone is an opioid antagonist used to reduce cravings in alcohol and opioid dependence.
Together, naltrexone and bupropion help regulate the brain’s reward system and hunger cues, making it easier for people to control food intake, resist emotional eating, and lose weight. Contrave is typically prescribed as part of a broader weight management strategy that includes a reduced-calorie diet, behavioral changes, and physical activity. However, these two medications can make Contrave drug interactions much more likely.
The medication is available in extended-release tablets to ensure consistent dosing throughout the day and minimize abrupt changes in blood concentration that could increase side effects.
What Is Nardil?
Nardil (phenelzine sulfate) is a monoamine oxidase inhibitor (MAOI) used to treat depression, particularly treatment-resistant or atypical forms that haven’t responded to SSRIs, SNRIs, or tricyclic antidepressants. MAOIs work by inhibiting the enzyme monoamine oxidase, which breaks down neurotransmitters like serotonin, dopamine, and norepinephrine. By blocking this enzyme, Nardil increases the levels of these neurotransmitters in the brain, improving mood and emotional stability.
However, MAOIs come with strict limitations due to their extensive and potentially dangerous drug interactions. They interact with numerous foods, over-the-counter medications, and other prescription drugs—especially those that also affect neurotransmitters.
These interactions can lead to severe complications, including extremely high blood pressure, serotonin syndrome, or hypertensive crisis, which is why careful oversight is required when prescribing or transitioning off an MAOI.
Why the Combination Is Risky
When you take naltrexone and bupropion together in Contrave, the bupropion component becomes a major concern if paired with MAOIs like Nardil. Both drugs influence dopamine and norepinephrine levels, and when combined, the resulting chemical overload can dangerously overstimulate the central nervous system.
The Most Serious Risks Include:
- Extremely high blood pressure: This can occur rapidly and may lead to stroke, heart attack, or other life-threatening cardiovascular events.
- Severe seizures: Bupropion already lowers the seizure threshold; pairing it with an MAOI further increases this risk, especially in patients with eating disorders, bipolar disorder, or a history of substance misuse.
- Sudden high body temperature: An early warning sign of serotonin syndrome or autonomic dysregulation.
- Pulse frequent urge changes: Fluctuations in heart rate or blood pressure may point to a developing crisis.
- Neck sweating vomiting rare symptoms: These may be part of a hypertensive reaction or early signs of neurological distress.
“There’s a boxed warning that alerts doctors about the increased risk of suicidal thoughts and behaviors when using naltrexone and bupropion in patients with mental disease or mood disorders,” says Dr. Matthew Olesiak. “Combining them with MAOIs further elevates that risk, particularly in vulnerable individuals.”
In addition to these serious risks, the combination of Contrave and Nardil may increase the risk of side effects such as:
- Discomfort, nausea, pain
- Serious skin reactions, including blistering or peeling
- Skin rash or hives
- Chest pain, agitation, or dizziness
- Low blood sugar or irregular blood sugar fluctuations in patients with diabetes
These effects are more likely in elderly patients or those with existing liver disease or kidney disease, where drug clearance is already compromised. Because both drugs are metabolized and excreted by these organs, toxic accumulation can occur quickly without close monitoring.
Potential Side Effects of Taking Contrave and Nardil Together
| Category | Possible Side Effects |
|---|---|
| Cardiovascular | High blood pressure, extremely high blood pressure, chest pain, rare chest pain, increased heart rate |
| Neurological | Severe seizures, severe spinning, nausea, headache, irritability, sudden or strong feelings |
| Psychiatric | Suicidal thoughts, mood changes, mental disease flare-ups, anxiety, agitation |
| Gastrointestinal | Discomfort, nausea, bowel symptoms, stomach pain, indigestion |
| Dermatological | Serious skin reactions, skin rash, severe acne, allergic reaction, skin reactions |
| Renal and Urinary | Common bladder pain, bloody, age-related kidney problems, end-stage kidney disease |
| Endocrine / Metabolic | Low blood sugar, fluctuations in blood sugar, weight changes |
| General / Systemic | Sudden high body temperature, neck sweating, vomiting rare, indigestion |
| Musculoskeletal | Sitting position muscle cramps, muscle tension, or weakness |
| Allergic / Immune Response | Allergic reaction, immediate medical attention required, accidental overdose |
Drug Interactions: What You Need to Know
MAOIs like Nardil are known to interact with a wide range of medications and substances, including naltrexone and bupropion, the two active ingredients in Contrave. This combination poses a serious risk due to overlapping mechanisms that affect neurotransmitters such as dopamine, norepinephrine, and serotonin.
What Can Happen When These Drugs Are Combined?
1. Increase blood pressure rapidly, sometimes to dangerous levels.
Combining bupropion with an MAOI can result in a hypertensive crisis—a sudden and extremely high blood pressure spike that may lead to stroke or cardiac complications. This occurs because both drugs elevate norepinephrine levels, which can overstimulate the cardiovascular system.
2. Trigger severe seizures.
Bupropion lowers the seizure threshold, particularly at higher doses or when combined with interacting drugs. When taken with an MAOI, this risk is amplified, especially in people with predisposing conditions like eating disorders, bipolar disorder, or a history of substance abuse.
3. Lead to suicidal thoughts or sudden or strong feelings.
The risk of suicidal thoughts is already heightened when taking naltrexone and bupropion, especially in young adults or people with mental illness. Adding an MAOI may intensify mood swings, emotional instability, or behavioral agitation.
4. Cause chest pain, agitation, or severe nausea.
People may experience a cluster of distressing symptoms such as rare chest pain, racing heart, dizziness, or severe nausea. These could indicate serotonin syndrome, autonomic instability, or other acute reactions that require immediate medical attention.
The U.S. Food and Drug Administration (FDA) provides specific guidelines regarding the interaction between monoamine oxidase inhibitors (MAOIs) and bupropion. According to the FDA, a minimum 14-day washout period should occur between discontinuing an MAOI intended to treat depression and starting therapy with bupropion. Conversely, at least 14 days should also elapse after stopping bupropion before initiating an MAOI. This washout period is necessary due to the increased risk of hypertensive reactions when bupropion is used concurrently with MAOIs.
“Even a single overlapping dose of Nardil and bupropion could lead to serious neurological or cardiovascular events,” warns Dr. Matthew Olesiak. “It’s not just about avoiding a bad reaction—it’s about preventing a true medical emergency.”
Side Effects to Watch For
Even if you’re not taking Contrave and Nardil together, being prescribed them close in time—or switching from one to the other—requires extra caution. These medications can cause overlapping or compounding side effects. Some may be mild at first, but others may signal a more serious issue developing under the surface.
Be Especially Alert For These Symptoms:
• Headache, irritability, and lack of energy
Often mistaken for fatigue or stress, these could be early signs of a reaction to naltrexone and bupropion, or signs your brain chemistry is being disrupted.
• Lips, stomach pain
This vague cluster can be a symptom of gastrointestinal upset, but when paired with skin flushing or chest pressure, it may indicate an early allergic reaction or autonomic issue.
• Allergic reaction (e.g., hives, swelling of the face, lips, or throat)
These reactions may seem minor at first but can escalate quickly into anaphylaxis. Seek immediate medical attention if you notice swelling, rashes, or trouble breathing.
• Bowel symptoms like nausea, vomiting, or diarrhea
Nausea is a common side effect of extended-release tablets, especially in the first weeks of starting Contrave treatment, but if paired with dizziness or frequent pulse issues, it may signal something more serious.
• Common bladder pain, bloody urine
Unusual urinary symptoms could point to an adverse renal reaction—especially in people with kidney disease or those taking high doses of naltrexone and bupropion.
• Chest pain or rare chest pain
Both medications can affect the heart. Any sensation of tightness, heaviness, or radiating pain in the chest should not be ignored, especially if you’re also feeling faint, dizzy, or nauseous.
If you experience any of the above, contact a medical professional immediately. These symptoms may indicate a severe risk of side effects, ranging from hypertensive crises to serotonin syndrome or even life-threatening reactions.
“No side effect should ever be dismissed as minor if it feels out of place for your body or your baseline,” notes Dr. Olesiak. “The key is to talk with your doctor early—before things escalate.”
Special Precautions
You should always talk with your doctor before starting Contrave treatment, stopping, or combining medications. This is critical to reduce the risk of side effects, particularly in individuals with preexisting health conditions or those taking other medications.
Here are some scenarios where increased risk is likely—and where extreme caution and medical oversight are required:
1. You Have Bipolar Disorder, Mental Disease, or a History of Suicidal Thoughts
People with mood disorders or mental disease, including bipolar disorder, are at greater risk for emotional instability and suicidal thoughts when taking naltrexone and bupropion.
These medications affect brain chemicals linked to mood regulation and can trigger sudden or strong feelings, mood swings, or even psychosis in sensitive individuals.
2. You Suffer from Liver Disease, Kidney Disease, or Age-Related Kidney Problems
Naltrexone and bupropion are metabolized by the liver and excreted through the kidneys. If you have liver disease, kidney disease, or age-related kidney problems, the drugs can build up in your system and lead to toxicity.
In these cases, your healthcare professional may need to adjust your dose or avoid Contrave altogether.
3. You Use Alcoholic Beverages or Drink Alcohol Regularly
Alcohol lowers the seizure threshold and may worsen side effects like dizziness, drowsiness, and nausea pain. It also increases the chances of experiencing accidental overdose or withdrawal-related symptoms if you’re taking naltrexone and bupropion to help reduce alcohol use.
“People with a history of alcohol abuse or dependency should be especially cautious,” says Dr. Matthew Olesiak. “Drink alcohol in moderation if at all, and never combine it with these medications unless cleared by your medical doctor.”
4. You Take Narcotic Drugs, Other Narcotic Medicine, or Other Habit-Forming Painkillers
Naltrexone is an opioid antagonist, meaning it blocks the effects of opioids. If you are taking narcotic drugs, other narcotic medicine, or other habit-forming painkillers, Contrave could cause sudden withdrawal symptoms or reduce the effectiveness of your pain medication.
You should never combine these without direct supervision by a healthcare professional.
5. You Have Eating Disorders Like Bulimia or Anorexia
Individuals with eating disorders often have electrolyte imbalances and a history of purging behaviors, which significantly increases the risk of severe seizures when taking bupropion, one of the active ingredients in Contrave.
This population is generally advised not to take Contrave due to the elevated seizure risk.
Drug Interactions to Watch For
Naltrexone and bupropion should not be taken with certain anxiety medicines (Xanax), antidepressant medications (Paxil, Lexapro, Effexor, Prozac, Cymbalta, Zoloft), over-the-counter sleep aids, or cold remedies containing stimulants (Ephedrine) or serotonin-affecting ingredients without the approval of your healthcare professional.
These combinations can lead to serious skin reactions, serotonin syndrome, or an increase in blood pressure.

Contrave Dosage and Safety Tips
Contrave comes as extended-release tablets, which are designed to maintain a steady release of naltrexone and bupropion in your system over time. According to the FDA-approved prescribing information, using these tablets as directed can reduce the risk of side effects and improve overall success in weight loss and weight management.
Here are key tips to ensure safe use:
Follow Your Doctor’s Instructions Carefully
Your medical doctor will start you on a gradually increasing dose to minimize side effects such as nausea pain, dizziness, or headaches. You should never adjust your dose on your own or take more than prescribed, even if you feel your progress has stalled.
“Many of the more severe issues we see stem from misuse,” warns Dr. Olesiak. “People often think more medication means faster weight loss, but it just increases the risk of complications.”
Never Take Double Doses If You Miss a Missed Dose
If you forget to take your dose, skip it and continue with your next scheduled one. Do not take double doses—taking extra to “make up” can trigger severe seizures, headache irritability lack, or confusion. Always follow your prescribed schedule.
Avoid High-Fat Meals
High fat meals can increase the absorption rate of bupropion, raising the chance of side effects like chest pain, discomfort nausea pain, or dizziness. Stick to a reduced calorie diet that supports your weight loss goals without compromising drug safety.
Sit or Stand Slowly
Some people may experience lightheadedness or muscle cramps in the sitting position when rising too quickly from sitting. This can be a result of fluctuating blood pressure, which is a known side effect of naltrexone and bupropion.
Should You Ever Take Contrave and Nardil Together?
In almost all cases, taking Contrave and Nardil together is not recommended due to the increased risk of life-threatening reactions. Most healthcare professionals will avoid prescribing them together unless absolutely necessary—and even then, only under tightly controlled conditions.
If you’re switching from one medication to another (e.g., stopping Nardil to begin starting Contrave treatment), you may need to wait 14–28 days, depending on your personal medical history.
Additional Safety Reminders
Even if you are following your prescribed dosage of Contrave, maintaining open communication with your healthcare team and staying vigilant about symptoms can help prevent serious complications.
Below are essential precautions to follow throughout your Contrave treatment, especially if you’re managing coexisting conditions or taking other medications.
1. Always Disclose Other Medicines or Other Medications You Take Regularly
Whether prescription, over the counter, or herbal supplements, every substance you take can potentially lead to certain drug interactions. Some may increase the risk of side effects, while others may reduce the effectiveness of naltrexone and bupropion.
Make a full list of all your other medications and share it with your healthcare professional at each appointment.
2. Notify Your Provider About Any Medical Tests You Have Scheduled
Both naltrexone and bupropion can interfere with lab test results, especially those measuring liver function or hormone levels.
Always talk with your doctor ahead of time if you have blood work, imaging, or any medical tests coming up, so they can advise you appropriately or adjust your treatment plan if needed.
3. Be Alert for Symptoms of Accidental Overdose
Taking too much Contrave—either intentionally or due to taking double doses after a missed dose—can lead to dangerous outcomes. Signs of an accidental overdose include tremors, severe seizures, confusion, blurred vision, and agitation.
These symptoms can escalate quickly and require immediate medical attention, so it’s vital to use the medication exactly as prescribed.
4. Don’t Mix Contrave with Narcotic Medicines Unless Your Medical Doctor Has Cleared It
Naltrexone, one of the active ingredients in Contrave, blocks the effects of opioids. If you’re taking narcotic medicines, narcotic drugs, or other narcotic medicines (codeine, methadone, morphine, fentanyl), combining them with Contrave could cause sudden withdrawal, intense pain, or a life-threatening reaction.
Your medical doctor must assess whether it’s safe for you to use Contrave in these circumstances.
5. Monitor Blood Sugar Closely, Especially if You Have Diabetes
Both naltrexone and bupropion can affect blood sugar regulation. You may experience episodes of low blood sugar, particularly if you’re on insulin or other glucose-lowering drugs. Keep a log of your blood sugar readings and report any unusual patterns to your healthcare professional.
Adjustments to your diabetes regimen or diet may be needed.
6. Report Any Skin Reactions or Severe Acne
Watch for signs of skin reactions, such as redness, blistering, rash, or severe acne. These could indicate an allergic reaction or even serious skin reactions that require stopping the medication.
If you notice any changes to your skin, no matter how minor, talk with your doctor right away.
7. Stay Hydrated and Monitor for Digestive Discomfort
Contrave may cause indigestion, nausea, or bloating, particularly during the early phases of treatment. Drinking enough water, eating smaller meals, and avoiding high-fat meals can help minimize symptoms like nausea, pain, stomach upset, or decreased appetite.
8. Use Contrave Only as Part of a Reduced Calorie Diet and Lifestyle Changes
Contrave is not a magic pill—it works best when combined with a reduced-calorie diet, increased physical activity, and healthy behavioral habits. If your goal is to lose weight or improve long-term weight management, following your full treatment plan is essential.
Taking Contrave without lifestyle changes may increase the risk of side effects without delivering the intended weight loss benefits.
Frequently Asked Questions (FAQ)
When it comes to prescription medications like Contrave and Nardil, understanding how they interact with other substances is key to staying safe.
Below are answers to some of the most common questions people ask about combining these drugs with other treatments, especially when managing weight loss, mood disorders, or chronic conditions.
1. What medications should not be taken with Contrave?
Several medications can interact dangerously with Contrave, especially those that affect the brain, liver, or blood pressure. Monoamine oxidase inhibitors (MAOIs) like Nardil must not be taken with Contrave due to the risk of extremely high blood pressure, severe seizures, and other life-threatening side effects.
In addition, narcotic drugs, other habit-forming painkillers, and drugs that lower the seizure threshold, like antipsychotics or certain anxiety medicines, can increase the risk of side effects. Over-the-counter products containing decongestants or stimulants may also raise blood pressure and should be avoided.
Always talk with your doctor before adding new medications while on Contrave.
2. What can you not take with Nardil?
Nardil is a powerful MAOI, and it comes with a long list of restricted substances. You should avoid all other antidepressants (especially SSRIs, SNRIs, and tricyclics), naltrexone and bupropion (found in Contrave), and any drugs that affect serotonin, dopamine, or norepinephrine.
Common cold medications, over-the-counter decongestants, and certain pain relievers like meperidine or tramadol can also cause serious skin reactions, serotonin syndrome, or dangerously high blood pressure. Even certain foods high in tyramine can trigger hypertensive episodes.
Because of these risks, it’s critical to talk with your doctor and review any other medications or supplements before using Nardil.
3. Can I take Contrave and Zoloft together?
Combining Contrave with Zoloft (sertraline), a selective serotonin reuptake inhibitor (SSRI), is not typically recommended without close medical supervision. Both medications influence brain neurotransmitters, and using them together may raise the risk of serotonin syndrome, severe seizures, and worsening mental disease symptoms like anxiety or suicidal thoughts. In some cases, a doctor may decide the benefits outweigh the risks, but this requires regular monitoring.
Be sure to talk with your doctor about any history of bipolar disorder, liver disease, or eating disorders, which may increase the likelihood of complications.
4. Can Contrave worsen depression?
Yes, Contrave can worsen symptoms of depression in some individuals, particularly those with a history of mood disorders or mental disease. The bupropion component is sometimes used to treat depression, but when combined with naltrexone, the emotional response can vary, especially during the initial weeks of treatment. There’s a boxed warning that alerts doctors about the possibility of suicidal thoughts, especially in young adults.
If you notice a change in mood, increased anxiety, or sudden or strong feelings, it’s important to talk with your doctor immediately. Monitoring and possible dosage adjustments can help reduce the risk of side effects.
Final Thoughts
The combination of Contrave and Nardil together can be dangerous without proper oversight. Given the potential for serious side effects, it’s crucial to talk with your doctor and follow up regularly.
“I advise patients to always keep an open line with their healthcare professional,” says Dr. Olesiak. “Even minor side effects can sometimes signal something bigger, especially with complex medications like naltrexone and bupropion or MAOIs.”
Always prioritize safety and long-term health outcomes over short-term weight loss goals. Remember, medications are tools—not substitutes for a broader weight management plan.
References
FDA Prescribing Information for Contrave.