Taking Contrave and Paxil Together Drug Interactions: a Good Idea?

Combining medications for weight loss and mental health can be beneficial in some cases, but it can also lead to serious complications if not managed carefully. One common concern is taking Contrave and Paxil together drug interactions.
Contrave is a prescription weight loss drug that contains bupropion hydrochloride and naltrexone, while Paxil (paroxetine) is an antidepressant used to treat depression, anxiety, and other mental health conditions.
While both medications can be helpful on their own, when taking Contrave and Paxil together, drug interactions between them may increase the risk of certain side effects, some of which may be severe. Understanding how these medications interact and how to use them safely is key to protecting both your mental and physical health.
Key Takeaways
- Taking Contrave and Paxil together may increase the risk of seizures, serotonin syndrome, and worsening of mental health conditions.
- Common side effects may be amplified, including high blood pressure, nausea, suicidal thoughts, and mood changes.
- Always consult your doctor or pharmacist before starting Contrave treatment, adjusting doses, or stopping either medication.
How Contrave Works: Active Ingredients and Effects
Contrave treatment combines two active ingredients: bupropion hydrochloride, an antidepressant and smoking cessation aid, and naltrexone, typically used to treat alcohol and opioid dependence. Together, these ingredients target areas of the brain involved in appetite and reward response, helping support long-term weight loss and weight management for compatible individuals.
Because bupropion hydrochloride is also used to treat depression, combining it with another antidepressant like Paxil increases the likelihood of certain drug interactions. These risks are detailed in the patient package insert and are critical to review before starting Contrave.
Paxil Overview: Mental Health Support and Risks
Paxil is a selective serotonin reuptake inhibitor (SSRI) often prescribed for depression, anxiety, panic attacks, and other mental health conditions. Like many other antidepressants, it alters neurotransmitter levels in the brain.
Using Paxil alongside bupropion, one of the active ingredients in Contrave, may affect serotonin and dopamine systems in ways that increase the risk of side effects. A 2004 case study published in Clinical Neuropharmacology documented a rare but serious instance of serotonin syndrome in a patient taking bupropion and an SSRI, highlighting the potentially life-threatening risks when these medications are combined (Munhoz, 2004).
Drug Interactions Between Contrave and Paxil
The combination of Contrave and Paxil together raises concern for several potential drug interactions, especially given the way each medication affects brain chemistry and cardiovascular function.
While both drugs may be prescribed individually to support weight loss or manage mental health conditions, using them in tandem can increase the risk of serious side effects. How does Contrave interact with Paxil?
Here are the most important risks to consider:
1. Increased Seizure Risk
One of the most well-documented risks of bupropion hydrochloride—a key active ingredient in Contrave—is its ability to lower the seizure threshold. Paxil, while less commonly associated with seizures, can further complicate this risk, particularly in patients with a history of seizure disorder, head trauma, or those who suddenly stop drinking alcohol.
Combining these medications can amplify the chances of seizure activity, especially if dosing is not carefully managed.
2. Elevated Blood Pressure
Both Contrave and Paxil have been associated with rises in blood pressure and heart rate. When used together, they may increase blood pressure to levels that are dangerous, particularly for individuals with preexisting high blood pressure or heart disease.
If you are already taking medications to treat high blood pressure, this interaction may reduce their effectiveness or worsen cardiovascular strain.
3. Worsening of Mental Health Symptoms
Since both drugs act on brain chemicals like serotonin, dopamine, and norepinephrine, combining them may destabilize mood in some individuals. This is especially true for people with bipolar disorder, who may experience manic episodes, or those with existing mental health problems, such as anxiety or PTSD.
The risk is higher during the initial weeks of therapy or during dosage changes.
4. Suicidal Thoughts or Behaviors
Like many antidepressants, Paxil carries a boxed warning that alerts doctors to the increased risk of suicidal thoughts, especially in adolescents and young adults. Bupropion, while often used to treat depression, can also contribute to mood instability in vulnerable individuals.
Taken together, the combined effect on emotional regulation and neurotransmitters may heighten this risk.
5. Serotonin Syndrome
Though rare, serotonin syndrome is a serious and potentially life-threatening condition caused by excess serotonin in the brain. Paxil increases serotonin levels directly, and while Contrave is not classified as an SSRI, bupropion can interfere with serotonin pathways indirectly.
Symptoms of serotonin syndrome include confusion, muscle rigidity, rapid heart rate, high fever, and tremors. Prompt medical attention is essential if these symptoms appear.
Dr. Matthew Olesiak, MD, Chief Medical Director at SANE MD, explains:
“When two drugs affect neurotransmitter systems—like bupropion and paroxetine—the overlap can disrupt balance and heighten side effects. Patients on both medications should be monitored closely, especially during the first weeks of combined treatment.”
These Contrave drug interactions are particularly concerning in individuals with a seizure disorder, bipolar disorder, or severely high blood pressure—all of which significantly increase the risk of complications when these medications are combined.
Why This Combination May Increase Side Effect Risks
Using both Contrave and Paxil can increase the risk of overlapping or amplified side effects because both medications directly impact the central nervous system. Each drug influences neurotransmitters that regulate mood, appetite, and stress responses.
When combined, their effects may interact in ways that the body isn’t equipped to handle, especially without careful monitoring.
Here’s how the risks can compound:
- Bupropion hydrochloride can increase blood pressure, and Paxil may also cause cardiovascular changes in some individuals. When used together, the risk of high blood pressure or rapid heart rate becomes more pronounced, which is particularly concerning in people with heart disease or those already taking medications to treat high blood pressure.
- Both medications affect mood and mental state, which may worsen mental health problems or trigger suicidal thoughts, especially in patients with a history of bipolar disorder, panic attacks, or other mental health conditions. Abrupt changes in dosage or inconsistent adherence can make these effects more unpredictable.
- Certain behaviors Contrave is designed to reduce—such as emotional or stress-related eating—can become harder to manage if Paxil dosing is altered. Since Paxil is a certain antidepressant that influences serotonin, any fluctuation in its effects may impact mood stability, appetite control, and weight management.
These overlapping drug effects can lead to a higher risk of side effects, particularly in the early stages of starting Contrave treatment, during dose changes, or when combining it with other antidepressants like Paxil. The FDA warns of such side effects in its patient labeling insert.
Common and Serious Side Effects to Watch For
When taking Contrave, especially in combination with Paxil or similar weight loss drugs, it’s important to be aware of both common and potentially serious reactions.
Many Contrave side effects result from the body adjusting to this drug’s active ingredients—bupropion hydrochloride and naltrexone—as well as the way those compounds may interact with other drugs that affect neurotransmitters, such as Paxil.
Side effects that may occur include:
- Increased blood pressure – May occur with either drug and should be closely monitored.
- Headache – Often reported during the first few weeks of Contrave treatment.
- Anxiety or mood swings – Can result from overstimulation or poor neurotransmitter balance.
- Dizziness – May be due to changes in blood pressure or drug effects on the brain.
- Nausea or vomiting – A common response when starting Contrave, especially without food.
- Low blood sugar – More likely in patients with diabetes; monitor levels regularly.
- Skin rash or signs of allergic reaction – Could indicate sensitivity to one of the active ingredients or other components of the medications.
- Difficulty sleeping – Often related to bupropion hydrochloride, especially when taken too late in the day.
- Tremors – Can be a sign of nervous system overstimulation.
- Visual changes – Blurred vision or visual distortion, though rare, should be reported immediately.
Dr. Matthew Olesiak, MD, emphasizes the importance of recognizing emotional shifts alongside physical symptoms:
“One of the most overlooked complications is the potential for Contrave to interfere with mental health stability. It’s not just about physical symptoms—emotional changes can be subtle at first but become dangerous quickly.”
If you experience warning signs of serotonin syndrome—such as high fever, muscle stiffness, confusion, rapid heart rate, or agitation—seek medical attention or call your local emergency number immediately.
This is a true medical emergency and must be addressed quickly to prevent complications.

Who Should Avoid Combining These Medications?
Some patients face a higher risk of Contrave interactions and should avoid this drug combination unless specifically guided by a provider.
Avoid combining these medications if you have:
- A seizure disorder or a history of head trauma
- Severely high blood pressure or uncontrolled heart disease
- History of bipolar disorder
- Active liver problems
- A history of eating disorders
- Mental health changes linked to medications
- Use of monoamine oxidase inhibitors (MAOIs) in the past 14 days
This combination may also be unsuitable for those who suddenly stop drinking alcohol, as bupropion can increase the risk of seizures during alcohol withdrawal.
Alcohol Use and Medication Safety
Patients who drink alcohol regularly or have recently stopped drinking alcohol should be cautious. Both Paxil and bupropion hydrochloride can increase the risk of seizures, and alcohol intensifies this effect.
For those who suddenly stop drinking alcohol, even a small dosage of Contrave may be dangerous.
It is essential to speak with your doctor or pharmacist before starting Contrave if alcohol is part of your lifestyle.
Blood Pressure and Heart Risks
One of the most important concerns with taking Contrave is the potential to increase blood pressure. When combined with Paxil—which may also affect cardiovascular responses—the risks can multiply. Other blood pressure medications, such as Lisinopril, Propranolol, and Losartan, may also negatively affect blood pressure when used with Contrave. Read more about Contrave hypertension risk in our detailed guide.
If you’re already taking medication to treat high blood pressure, your provider may recommend extra monitoring or adjustments. High blood pressure and heart rate may go unnoticed at first, but can increase the risk of cardiovascular events if left unmanaged.
Other Medications and Hidden Risks
In addition to Paxil, Contrave may interact with many other medications, including:
- Other antidepressants
- Certain beta blockers
- Over-the-counter cold remedies
- Drugs that affect liver enzymes
- Vitamins and supplements (e.g., vitamin interactions)
Be cautious of other drugs you may be taking, even if they seem unrelated. Some weight loss treatments, hormonal medications, or even lab tests may be affected by Contrave. A false positive result on drug tests is also possible when taking Contrave.
Always inform your provider of your health history, including any health conditions, mental health problems, or previous medication reactions.
What to Discuss With Your Doctor or Pharmacist
Before you begin Contrave treatment, it’s important to have an open and thorough conversation with your doctor or pharmacist.
This helps ensure the medication is safe for your individual needs and reduces the chance of dangerous drug interactions or unexpected side effects.
Be sure to discuss:
- All other medications you’re taking: This includes prescriptions, over-the-counter drugs, and recent treatments. Some other medications, including antidepressants, seizure medications, and certain blood pressure drugs, may interact with Contrave or increase the risk of adverse reactions.
- Any known allergic reactions: Let your provider know if you’ve ever had a skin rash, difficulty breathing, or any other allergic reaction to medications, especially bupropion, naltrexone, or similar compounds.
- Your history of heart disease, liver problems, or bipolar disorder: These health conditions can affect how your body handles Contrave and may increase the risk of complications like high blood pressure, mood swings, or liver strain.
- Whether you’re pregnant, breastfeeding, or planning to become pregnant: Since Contrave passes into breast milk, it may not be recommended for use while nursing or during pregnancy. Your doctor can help weigh the risks and benefits based on your situation.
- If you’re using any over-the-counter supplements or natural products: Herbal products, vitamins, or over-the-counter supplements can cause vitamin interactions or interfere with Contrave’s effects. Even seemingly harmless items like caffeine pills or St. John’s Wort can pose a risk.
This conversation is essential for tailoring your weight loss treatment safely and effectively. It helps your provider make informed decisions and minimizes your risk of side effects—especially if you’re also managing other health conditions or taking other drugs.
Tips for Taking Contrave Safely
Taking Contrave can support long-term weight loss and weight management, but it’s important to use the medication carefully to reduce your risk of side effects and avoid serious drug interactions.
Whether you’re using Contrave on its own or with medications like Paxil, following safety guidelines is essential.
Here are key safety tips:
- Never combine with monoamine oxidase inhibitors (MAOIs): Taking Contrave with MAOIs—such as phenelzine or tranylcypromine—can cause dangerous spikes in blood pressure or trigger serotonin syndrome. Wait at least 14 days after stopping an MAOI before starting Contrave treatment.
- Avoid high-fat foods, which may increase side effects: Meals high in fat can boost the absorption of Contrave too quickly, increasing the likelihood of nausea, vomiting, and other side effects. Stick to balanced, low-fat meals while on Contrave treatment to help your body tolerate the medication.
- Don’t abruptly stop or start either medication without guidance: Suddenly discontinuing Contrave or other medications like antidepressants may lead to withdrawal symptoms, mood changes, or increased seizure risk. Always consult your doctor or pharmacist before making changes to your treatment plan.
- Monitor your blood pressure regularly: Contrave may increase blood pressure and heart rate, especially during the early stages of use. If you already treat high blood pressure, your provider may need to adjust your treatment or monitor your cardiovascular health more closely.
- Report any signs of allergic reaction or mental health changes: Be alert for signs like rash, itching, swelling, or changes in mood, behavior, or thoughts. These could signal an allergic reaction, worsening mental health problems, or rare but serious side effects like suicidal thoughts.
In addition:
- Be consistent with your weight loss and weight management goals by following your provider’s full plan, including dietary guidance and physical activity.
- Remember that Contrave comes in extended-release tablets—they must be swallowed whole. Do not cut, crush, or chew them, as this can release the medication too quickly and increase the risk of side effects.
Frequently Asked Questions (FAQ)
When it comes to combining medications for weight loss, mood regulation, or chronic conditions, safety is key. Many patients taking Contrave, Paxil, or both have questions about possible drug interactions and how to manage their prescriptions without increasing their risk of side effects.
Below are answers to some of the most common concerns about Contrave interactions, antidepressants, and safe medication use.
1. What drugs cannot be taken with Paxil?
Paxil (paroxetine) should not be combined with monoamine oxidase inhibitors (MAOIs), including drugs like phenelzine or selegiline, due to the risk of serotonin syndrome, which can be life-threatening. Other medications to avoid include pimozide, thioridazine, and certain NSAIDs or blood thinners, which may increase the risk of bleeding. Caution is also advised when taking other SSRIs, SNRIs, or certain beta blockers.
Always consult your doctor or pharmacist before adding any other medications, including over-the-counter products or supplements, to avoid potentially serious drug interactions.
2. Can you take bupropion and Paxil together?
Yes, bupropion (an active ingredient in Contrave) and Paxil are sometimes prescribed together, but the combination can pose risks. Because both drugs influence neurotransmitters in the brain, taking them at the same time may increase the risk of seizures, mental health changes, and suicidal thoughts in certain individuals.
Close monitoring is especially important when starting treatment, adjusting doses, or if the patient has a history of mental health conditions like bipolar disorder or panic attacks. This combination should only be used under medical supervision.
3. Can you take Contrave with Paxil?
Taking Contrave with Paxil is possible but comes with important safety considerations. Since Contrave contains bupropion hydrochloride, it can interact with Paxil to increase the chances of high blood pressure, seizure disorder symptoms, and serotonin-related side effects.
Both medications can also affect mood, which may trigger mental health problems or emotional instability in sensitive individuals. This combination is not uncommon, but it requires careful dose management and regular check-ins with a healthcare provider.
4. What medications should not be taken with Contrave?
Contrave should not be taken with monoamine oxidase inhibitors (MAOIs), other bupropion-containing drugs, or medications that can increase the risk of seizures, such as certain antipsychotics, stimulants, and corticosteroids.
It’s also important to avoid using Contrave with opioids or drugs used to treat opioid dependence, as naltrexone can block their effects. People who have recently suddenly stopped drinking alcohol or taking benzodiazepines should avoid Contrave due to seizure risk.
Tell your doctor about all other medications, including over-the-counter products and supplements, to prevent harmful drug interactions.
5. Can you take Contrave while on antidepressants?
In some cases, yes—Contrave treatment may be combined with certain antidepressants, but it depends on the specific medication and the individual’s health history. Combining Contrave with SSRIs like Paxil may increase the risk of side effects such as suicidal thoughts, mood swings, and high blood pressure.
These risks are higher in people with mental health conditions, bipolar disorder, or a history of drinking alcohol heavily. If your provider decides to prescribe Contrave alongside an antidepressant, you’ll need careful dose adjustments and monitoring to minimize adverse effects.
Final Thoughts on Contrave and Paxil Together
Combining Contrave and Paxil together can be risky, but it’s not always unsafe—especially under close supervision. Still, it’s critical to understand the risk of side effects, monitor your mental health, and work with a trusted healthcare provider.
While Contrave may offer benefits for weight loss, especially in patients with obesity or related health conditions, it’s not for everyone. The combination with Paxil requires caution, monitoring, and a personalized approach.
If you experience troubling side effects, seek medical advice promptly. When in doubt, call your doctor, pharmacist, or your local emergency number if you suspect a serious reaction.
References

Celexa and Contrave Drug Interactions: What to Know

Celexa (citalopram) and Contrave (bupropion-naltrexone) are medications used for different purposes—Celexa to treat depression and Contrave for chronic weight management for compatible individuals.
However, Celexa and Contrave drug interactions can occur if these two medications are taken together, affecting safety and efficacy. Understanding these risks is essential before combining these medications.
Key Takeaways
- Celexa and Contrave drug interactions can increase the risk of serious adverse reactions such as seizures and high blood pressure.
- Taking Contrave with Celexa may require dose adjustment to minimize the risk of seizures and other side effects.
- Patients with bipolar disorder, a seizure disorder, eating disorders, or other risk factors should consult their doctor before taking these medications together.
Understanding Celexa and Contrave Drug Interactions
Celexa (citalopram) is a selective serotonin reuptake inhibitor (SSRI) commonly prescribed to treat depression and other mood disorders. It works by increasing serotonin levels in the brain, improving mood regulation and emotional stability. Contrave, on the other hand, is a weight loss medication that combines naltrexone and bupropion to influence appetite and cravings by acting on the brain’s reward system. Naltrexone is an opioid antagonist used to treat alcohol and opioid dependence, while bupropion is an atypical antidepressant that affects dopamine and norepinephrine levels. Contrave helps promote weight loss in certain individuals.
When Celexa and Contrave are taken together, their interaction can have unintended effects due to the way both medications alter neurotransmitter activity. Bupropion, a key component of Contrave, inhibits the reuptake of dopamine and norepinephrine, while Celexa primarily affects serotonin. The combination can create an imbalance in neurotransmitter regulation, increasing the likelihood of adverse reactions such as serotonin syndrome, nervous system overstimulation, and mood instability.
One of the most significant concerns with this combination is the lower seizure threshold caused by bupropion. Since Celexa may also contribute to mild excitatory effects in the nervous system, the concurrent use of these drugs increases the risk of seizures, particularly in individuals with a history of seizure disorder, bipolar disorder, or brain trauma.
Dr. Matthew Olesiak, MD, Chief Medical Director of SANE MD, states:
“Bupropion, a key ingredient in Contrave, is known to reduce seizure threshold. When combined with an SSRI like Celexa, the risk of seizures may further increase, especially in patients with preexisting risk factors.”
In addition to seizure risk, the interaction between Celexa and Contrave can contribute to serotonin syndrome, a potentially life-threatening condition characterized by confusion, rapid heart rate, high blood pressure, sweating, muscle stiffness, and agitation. This occurs when excessive serotonin accumulates in the nervous system, often as a result of combining multiple drugs that influence serotonin levels.
Celexa and Contrave Drug Interaction Summary
| Category | Details |
|---|---|
| Primary Medications | – Celexa (Citalopram): SSRI antidepressant increasing serotonin levels – Contrave: Weight loss drug (naltrexone + bupropion) acting on dopamine/norepinephrine |
| Main Interaction Concerns | – Increased seizure risk due to bupropion – Risk of serotonin syndrome – Blood pressure elevation – CNS overstimulation |
| High-Risk Groups | – Individuals with: – Seizure disorders – Bipolar disorder – Brain injuries – Eating disorders |
| Neurological Side Effects | – Dizziness or vertigo – Confusion or poor concentration – Tremors or twitching – Insomnia or restlessness – Blurred vision |
| Cardiovascular Risks | – High blood pressure – Severe headaches – Chest pain or palpitations – Shortness of breath |
| Opioid Interaction Risks | – Naltrexone blocks opioid receptors – May cause withdrawal if taken with opioids – Risk of overdose after stopping Contrave and resuming opioids |
| Suicidal Thoughts Risk | – Both drugs can increase suicidal ideation, especially in those <25 – Watch for sudden mood changes, aggression, or withdrawal |
| Serious Allergic Reactions | – Rash or hives – Dark urine (possible liver issue) – Chest pain or difficulty breathing |
Increased Risk of Seizures and CNS Toxicity
Taking Contrave with Celexa can significantly increase the risk of seizures, especially for individuals who have a seizure disorder, bipolar disorder, a history of traumatic brain injury, or a brain tumor. According to research published in Pharmacy & Therapeutics Journal, Bupropion, one of the main components of Contrave, is known to lower seizure threshold, making seizures more likely when combined with other medications that impact the central nervous system (CNS), such as Celexa.
Additionally, naltrexone and bupropion both influence neurotransmitter activity in the brain, which can contribute to CNS toxicity when taken with Celexa. This may lead to symptoms such as:
- Dizziness or vertigo
- Confusion or difficulty concentrating
- Tremors or muscle twitching
- Increased nervous system stimulation, leading to restlessness or insomnia
- Headaches and blurred vision
Because these side effects can affect cognitive function, patients should avoid activities requiring mental alertness, such as driving or operating heavy machinery, until they fully understand how the combination of medications affects them.
Dr. Olesiak notes: “Patients taking both Celexa and Contrave should be cautious of potential neurological side effects, including dizziness and tremors, which may impair motor function and decision-making.”
In individuals predisposed to seizures, even small changes in dosage or missed doses can trigger an episode. The FDA emphasizes the importance of following a healthcare provider’s guidance on dose adjustments to minimize the risk of seizures.
Blood Pressure and Cardiovascular Concerns
Both Celexa and Contrave can impact blood pressure, but taking Contrave increases the likelihood of developing high blood pressure or severely high blood pressure, particularly in individuals who have preexisting cardiovascular conditions. Bupropion, a stimulant-like drug, can elevate blood pressure, while naltrexone can also contribute to fluctuations in heart rate and blood pressure or heart function.
Patients who already have hypertension, heart disease, or a history of stroke are at an even higher risk of developing hypertensive reactions, which may present as:
- Severe headaches
- Dizziness and vision changes
- Chest pain or palpitations
- Shortness of breath
For individuals on both Celexa and Contrave, frequent monitoring of blood pressure is essential to prevent dangerous spikes.
Dr. Olesiak advises: “Because bupropion can cause an increase in blood pressure, patients taking Contrave should regularly monitor their readings, especially if they are also on SSRIs like Celexa.”
If a patient develops severely high blood pressure or experiences chest pain, they should seek immediate medical attention. In some cases, a dose adjustment or alternative treatment may be necessary to lower the risk of cardiovascular complications.
Additional Risks and Considerations
Opioid Withdrawal & Accidental Overdose
Since naltrexone and bupropion block opioid receptors, individuals using opioid-based medications or struggling with opioid dependence must avoid taking Contrave. This is because naltrexone prevents opioids from binding to receptors, which can trigger opioid withdrawal symptoms if the individual is physically dependent.
Common symptoms of opioid withdrawal include:
- Severe nausea and vomiting
- Sweating and chills
- Increased heart rate and blood pressure
- Muscle aches and restlessness
Additionally, individuals who stop taking Contrave and later use opioids may have a reduced tolerance, making them susceptible to an accidental overdose, which could be fatal. Patients should tell their doctor if they are taking opioids before starting Contrave treatment.
Increased Risk of Suicidal Thoughts
As with most antidepressants, Celexa carries an FDA warning for suicidal thoughts in young adults, particularly during the initial weeks of treatment. Bupropion, while not a traditional SSRI, also alters brain chemistry, and its stimulating effects may increase the risk of anxiety, restlessness, or impulsivity. When used together, these drugs may elevate the likelihood of:
- Suicidal ideation
- Self-harm thoughts
- Severe mood swings or aggression
Patients (especially those under the age of 25) and their families should monitor for behavioral changes, including sudden agitation, social withdrawal, or unexplained mood shifts. Tell your doctor immediately if these symptoms occur.
Serious Allergic Reaction
Though uncommon, some individuals may experience a serious allergic reaction to Celexa, Contrave, or their combined effects.
Symptoms of a severe allergic reaction include:
- Skin rash or hives
- Dark urine, indicating possible liver issues
- Severe chest pain or difficulty breathing
If any of these symptoms occur, seek immediate medical attention to prevent serious complications. Tell your doctor about any history of allergies before taking these medications.
Understanding these side effects and safety guidelines can help you take these medications safely.
Safe Use Guidelines
To reduce the potential risks associated with Celexa and Contrave drug interactions, patients should follow these essential safety guidelines:
1. Tell Your Doctor About All Other Drugs and Over-the-Counter Drugs You Are Taking
Many other drugs, including over-the-counter drugs, herbal supplements, and prescription medications, can interact with Celexa and Contrave, potentially increasing the risk of adverse reactions.
Some medications that require special attention include:
- Other antidepressants (e.g., SSRIs, SNRIs, MAOIs)
- Antipsychotic medications (may further lower seizure threshold)
- Blood pressure medications (as Contrave may cause fluctuations in blood pressure)
- Opioid pain relievers, Codeine such as , (which Contrave blocks due to its naltrexone component)
- Over-the-counter drugs like decongestants or nonsteroidal anti-inflammatory drugs (NSAIDs), which may elevate blood pressure
Additionally, stimulants like Modafinil can also interact with Contrave.
Since some interactions may increase the risk of seizures, hypertensive reactions, or serotonin syndrome, it is critical to tell your doctor about all medications you are taking before starting Contrave treatment.

2. Avoid High-Fat Meals When Taking Contrave
Taking Contrave with high-fat meals can increase systemic exposure to bupropion, leading to a higher risk of adverse effects, including:
- Increased blood pressure or heart rate
- Nausea, dizziness, or agitation
- Lower seizure threshold, heightening the risk of seizures
To minimize these risks, Contrave tablets should be taken with a reduced-calorie diet, but without excessive dietary fat.
Patients should focus on balanced meals and avoid consuming high-fat meals around their dosing schedule.
3. Do Not Suddenly Stop Drinking Alcohol
Abruptly stopping alcohol consumption while taking Contrave or Celexa can increase the risk of withdrawal symptoms, including:
- Seizures (due to bupropion lowering seizure threshold)
- Severe agitation or anxiety
- Sleep disturbances and mood instability
However, if you’re not a regular drinker, you should avoid drinking alcohol while on either of these drugs. (Contrave and alcohol drug interactions can be particularly severe.)
Patients who regularly consume alcohol should discuss a safe reduction plan with their healthcare provider before starting Contrave treatment.
Tell your doctor if you have a history of heavy alcohol use, as you may require a dose adjustment or closer monitoring.
4. Swallow Contrave Tablets Whole—Do Not Crush, Chew, or Split Them
Contrave tablets are extended-release tablets, meaning the medication is designed to be released into the body gradually over time.
Crushing, chewing, or splitting the tablets can:
- Cause a sudden spike in drug levels, leading to adverse reactions
- Increase the risk of seizures, particularly in individuals predisposed to them
- Alter how the medication is absorbed, reducing effectiveness
Patients should swallow Contrave tablets whole with water and follow the prescribed dosing schedule. If a dose is missed, take the next scheduled dose rather than doubling up.
5. Follow the Prescribed Dose Range and Take Contrave in Divided Doses
To minimize the risk of hypertensive reactions, seizures, and other side effects, Contrave should be taken exactly as prescribed. Typically, Contrave is started at a lower dose and gradually increased to help the body adjust.
Taking too much too quickly can increase the risk of:
- Severely high blood pressure (Combining Contrave with Propranolol, a beta-blocker, can further affect blood pressure.
- Nervous system overstimulation (e.g., restlessness, jitteriness)
- Lower seizure threshold, increasing seizure risk
Patients should never exceed the recommended dose range or change their dosing schedule without consulting a healthcare provider.
6. Monitor for Trouble Sleeping, as Contrave Can Cause Insomnia
Contrave contains bupropion, a stimulant-like drug, which can cause trouble sleeping, particularly if taken too close to bedtime.
Patients who experience persistent insomnia should:
- Take Contrave earlier in the day to reduce its impact on sleep
- Avoid caffeine and other stimulants, which may worsen restlessness
- Discuss potential dose adjustments with their doctor if sleep disturbances become severe
If insomnia persists, tell your doctor, as alternative treatment strategies may be needed to ensure safe and effective chronic weight management without disrupting sleep quality.
FAQ: Celexa and Contrave Drug Interactions
When considering Celexa and Contrave drug interactions, it’s important to understand how these medications may interact with each other and with other drugs. Both Celexa (citalopram) and Contrave (naltrexone-bupropion) affect neurotransmitters, meaning their combination can lead to an increased risk of side effects, including seizures, high blood pressure, and serotonin syndrome.
Below are answers to some of the most common questions regarding their safe use.
1. Can you take Contrave while on antidepressants?
Taking Contrave while on antidepressants can be risky due to potential interactions between bupropion (a component of Contrave) and other antidepressants. Bupropion can increase serotonin and dopamine levels, which, when combined with SSRIs or SNRIs, may raise the risk of serotonin syndrome—a dangerous condition characterized by agitation, rapid heartbeat, and high fever.
Additionally, bupropion can lower the seizure threshold, making seizures more likely, especially if combined with medications that have similar effects. Patients currently on antidepressants should consult their doctor before starting Contrave, as a dose adjustment or alternative treatment may be necessary.
2. Can Celexa and buPROPion be taken together?
Celexa (citalopram) and bupropion are sometimes prescribed together, but this combination requires careful monitoring. While both medications are used to treat depression, they act on different neurotransmitters—Celexa primarily affects serotonin, while bupropion impacts dopamine and norepinephrine. Taking them together may increase the risk of seizures, especially in patients with seizure disorder, bipolar disorder, or other neurological conditions. There is also a potential for high blood pressure or mood instability.
If these medications are prescribed together, patients should be monitored for trouble sleeping, restlessness, and changes in blood pressure. Always tell your doctor about any side effects that arise.
3. What medications should not be taken with Contrave?
Several medications should not be taken with Contrave due to the risk of severe drug interactions.
These include:
- Opioid medications (e.g., oxycodone, morphine, fentanyl) – Contrave contains naltrexone, which blocks opioid receptors, potentially causing opioid withdrawal if taken together.
- Monoamine oxidase inhibitors (MAOIs) (e.g., phenelzine, selegiline) – These drugs can lead to dangerous blood pressure spikes and serotonin syndrome when combined with Contrave.
- Other drugs that lower seizure threshold (e.g., antipsychotics, steroids, certain antibiotics) – Combining them with Contrave may increase the risk of seizures.
- Stimulants and amphetamines (e.g., Adderall, Ritalin) – These can exacerbate Contrave’s effects on blood pressure and the central nervous system, increasing the likelihood of hypertension, anxiety, or heart issues.
Because Contrave contains bupropion and naltrexone, it’s crucial to tell your doctor about all other drugs and over-the-counter medications you’re taking.
4. What Cannot be taken with Celexa?
Several medications should not be taken with Celexa due to the risk of dangerous interactions.
These include:
- Other antidepressants, especially MAOIs – Combining Celexa with MAOIs or other SSRIs/SNRIs can lead to serotonin syndrome, a life-threatening condition.
- NSAIDs and blood thinners (e.g., aspirin, warfarin) – Celexa can increase the risk of bleeding, particularly in patients using blood thinners.
- Certain heart medications – Drugs that prolong the QT interval (e.g., amiodarone, sotalol) can increase the risk of irregular heart rhythms when taken with Celexa.
- St. John’s Wort – This herbal supplement can increase serotonin levels, heightening the risk of serotonin syndrome.
Patients should always tell their doctor about all medications and supplements they are taking before starting Celexa.
5. Can you take citalopram with Contrave?
Taking citalopram (Celexa) with Contrave can be dangerous due to their combined effects on neurotransmitters and blood pressure. Bupropion in Contrave lowers the seizure threshold, while citalopram can prolong the QT interval, increasing the risk of serious heart rhythm issues. Additionally, both drugs impact serotonin levels, which may increase the risk of serotonin syndrome if taken together.
Patients with a history of seizures, heart conditions, or high blood pressure should avoid taking these medications together unless advised by their doctor. If prescribed both, close monitoring of blood pressure, heart function, and neurological symptoms is essential to reduce the risk of serious side effects.
Conclusion
The Contrave interactions with Celexa pose risks that require careful monitoring. Individuals considering this combination should consult a healthcare professional to determine if a dose adjustment is needed or if alternative medications should be considered. Tell your doctor immediately if experiencing severe hepatic impairment, eye pain, or signs of an allergic reaction.
Understanding these interactions before starting Contrave treatment is crucial to ensuring a safe and effective treatment regimen for chronic weight management while minimizing the risk of seizures and high blood pressure.
References
Pharmacy & Therapeutics Journal

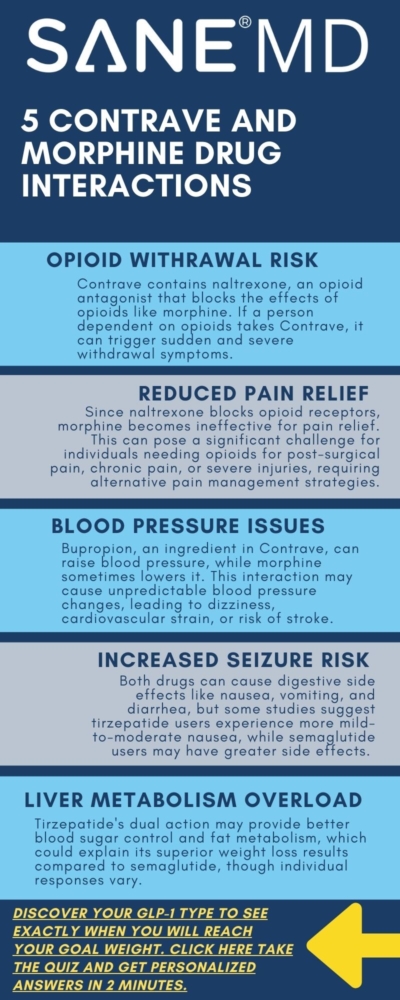
Contrave and Morphine Drug Interactions: What to Know

Understanding the potential Contrave and morphine drug interactions is crucial for individuals managing weight loss while requiring pain management. Contrave is a prescription medication combining naltrexone and bupropion, approved for chronic weight management in certain adults with an initial body mass index (BMI) of 30 kg/m² or greater or 27 kg/m² with at least one weight-related comorbidity. Morphine is a potent opioid analgesic used to treat severe pain.
Combining these medications can lead to significant drug interactions, primarily due to naltrexone’s role as an opioid antagonist, which can precipitate opioid withdrawal and affect pain management efficacy.
Dr. Matthew Olesiak, Chief Medical Director at SANE MD, emphasizes, “Patients must inform their healthcare providers about all medications they are taking, including over-the-counter drugs and supplements, to prevent adverse interactions between Contrave and opioid medications like morphine.”
Key Takeaways
- Naltrexone, a component of Contrave, can block the effects of opioids like morphine, potentially leading to opioid withdrawal symptoms.
- Both naltrexone and bupropion can influence blood pressure, necessitating careful monitoring when combined with other medications affecting cardiovascular health.
Comprehensive communication with a healthcare provider is essential to manage potential interactions and ensure safe medication use.
Medication Guide
Before starting Contrave treatment, patients should carefully review the medication guide provided by their healthcare provider or pharmacist. The medication guide contains important details about how to take Contrave, potential drug interactions, and possible adverse reactions.
It is essential to follow the guidelines outlined in the medication guide to avoid serious complications, such as opioid withdrawal, high blood pressure, or serotonin syndrome. If there are any concerns or questions about the medication guide, patients should consult their healthcare provider for clarification.
Contrave and Morphine Drug Interaction Table
| Interaction | Effect | Recommendation |
|---|---|---|
| Opioid Withdrawal | Naltrexone in Contrave blocks opioid receptors, leading to withdrawal symptoms if opioids like morphine are used. | Avoid opioid use while taking Contrave. Detox from opioids for at least 7-10 days before starting Contrave. |
| Reduced Pain Management | Naltrexone blocks the pain-relieving effects of morphine, making it ineffective. | Use non-opioid alternatives such as acetaminophen or NSAIDs for pain relief. |
| Blood Pressure Variations | Bupropion in Contrave can increase blood pressure, while morphine may lower it, causing unpredictable fluctuations. | Monitor blood pressure regularly and consult a healthcare provider if fluctuations occur. |
| Increased Seizure Risk | Bupropion lowers seizure threshold, and opioid withdrawal may increase seizure risk. | Avoid alcohol, sudden discontinuation of Contrave, and other seizure-inducing medications. |
| Liver Health Concerns | Both Contrave and morphine are metabolized in the liver, potentially increasing toxicity risk in individuals with liver disease. | Regular liver function tests are recommended for patients with liver conditions. Avoid high-fat meals while on Contrave. |
| Medication Alternatives | Morphine is ineffective while taking Contrave due to naltrexone’s opioid blockade. | Consider non-opioid pain relief options such as NSAIDs, acetaminophen, or nerve pain medications like gabapentin. |
| Emergency Pain Management | Contrave blocks opioid efficacy, making emergency pain relief difficult. | Inform healthcare providers about Contrave use before surgeries or procedures requiring opioids. Temporary discontinuation of Contrave may be necessary. |
What Is Contrave?
Contrave is a prescription medication approved for chronic weight management in adults with an initial body mass index (BMI) of 30 or higher, or 27 or higher with weight-related conditions such as high blood pressure or type 2 diabetes. It combines naltrexone and bupropion, two drugs that work together to help compatible patients lose weight when used alongside a reduced-calorie diet and physical activity.
- Naltrexone is an opioid antagonist primarily used to treat alcohol and opioid dependence. In Contrave, it plays a role in reducing food cravings.
- Bupropion is an antidepressant that helps regulate appetite and energy balance. It is also used to treat depression and aid in smoking cessation.
Taking Contrave requires medical supervision, especially for individuals with high blood pressure, mental illness, or a history of eating disorders such as anorexia nervosa.
The medication is available in the form of extended-release tablets. It is important to avoid using it if you have taken monoamine oxidase inhibitors (MAO inhibitors) within the last two weeks.
What Is Morphine?
Morphine is a powerful opioid medication prescribed to treat pain, particularly severe pain that does not respond to other pain relievers. It works by binding to opioid receptors in the brain and spinal cord, reducing the perception of pain.
Morphine is available in various forms, including extended-release and immediate-release tablets, as well as injectable and liquid formulations. While effective for pain management, morphine use carries risks, including dependence, tolerance, and opioid withdrawal symptoms if suddenly discontinued.
Patients with liver disease, renal impairment, or head injury should use morphine with caution. Additionally, combining morphine with other central nervous system depressants, including alcohol, can lead to trouble breathing and life-threatening complications. Individuals using morphine should follow their healthcare provider’s guidance to minimize the risk of serious injury or overdose.
How Contrave and Morphine Affect the Body
Contrave is used for chronic weight management in certain individuals with an initial body mass index (BMI) above a certain threshold. It combines naltrexone and bupropion, where naltrexone is an opioid antagonist, and bupropion is an antidepressant that may treat depression and help with weight loss. Morphine, on the other hand, is a severe pain reliever belonging to the opioid medications class.
When taking Contrave, patients should avoid opioids, including morphine, as naltrexone can block their effects, rendering them ineffective and leading to opioid withdrawal. Additionally, both medications can elevate blood pressure, increasing the increased risk of chest pain and cardiovascular morbidity.
Mechanism of Action: Contrave and Morphine
Contrave combines two active ingredients:
- Naltrexone: An opioid antagonist that blocks opioid receptors, reducing the rewarding effects of alcohol and opioids.
- Bupropion: An aminoketone antidepressant that inhibits the reuptake of norepinephrine and dopamine, neurotransmitters involved in regulating mood and appetite.
Together, these components target central nervous system pathways to aid in weight management.
Morphine is an opioid analgesic that binds to opioid receptors in the brain and spinal cord to alleviate pain. However, when naltrexone is present, it can block these receptors, rendering morphine less effective or ineffective. This antagonistic action can precipitate opioid withdrawal symptoms in individuals dependent on opioids.
Potential Risks of Combining Contrave and Morphine
1. Opioid Withdrawal
Administering naltrexone to individuals dependent on opioids like morphine can induce acute withdrawal symptoms, which may be severe and require immediate medical attention. Because naltrexone is an opioid antagonist, it rapidly displaces opioids from their receptors, leading to sudden and intense withdrawal effects.
Symptoms may include severe nausea, vomiting, sweating, tremors, rapid heartbeat, high blood pressure, agitation, confusion, and intense cravings. In extreme cases, withdrawal can lead to dehydration, cardiovascular instability, or seizures, requiring hospitalization.
Individuals who have been on long-term opioid therapy should not take Contrave unless they have fully detoxed from opioids for at least 7-10 days, as recommended by the FDA. Even in patients who are not opioid-dependent, taking Contrave after recent opioid use (such as post-surgical morphine administration) can trigger partial withdrawal symptoms, leading to discomfort and distress.
2. Altered Pain Management
Because naltrexone blocks opioid receptors, it can significantly reduce the analgesic effects of morphine and other opioid medications. This poses a serious challenge for individuals managing chronic pain, post-surgical recovery, or acute injuries requiring opioid analgesia. If a patient taking Contrave needs pain relief, alternative non-opioid pain management strategies, such as acetaminophen, NSAIDs (like ibuprofen or naproxen), or nerve pain medications (such as gabapentin), should be considered.
However, naltrexone’s effects on opioid receptors can last for up to 24 hours, meaning that even if opioid medications are later introduced, they may not work effectively until naltrexone has cleared the body. For individuals needing emergency or post-surgical opioid pain management, tell your doctor about taking Contrave in advance so proper pain relief strategies can be planned.
3. Blood Pressure Variations
Bupropion, one of the active ingredients in Contrave, is known to increase blood pressure and heart rate, potentially leading to high or severely high blood pressure in susceptible individuals (FDA).
Since morphine can sometimes cause low blood pressure, the combination of these two drugs may create unpredictable blood pressure fluctuations, putting additional strain on the cardiovascular system.
Patients with pre-existing hypertension, cardiovascular disease, or a history of stroke are at increased risk of complications. Tell your doctor before taking Contrave if you have high blood pressure or any other cardiovascular morbidity to ensure appropriate monitoring.
Blood pressure should be regularly checked while on Contrave treatment, and adjustments to medication or lifestyle factors (such as a reduced calorie diet and physical activity) may be required.
4. Seizure Risk
Bupropion is known to lower the seizure threshold, meaning that individuals taking Contrave are at an increased risk of seizures, particularly if they have predisposing conditions such as a history of seizures, head injury, or eating disorders like anorexia nervosa or bulimia nervosa. (NIH).
Additionally, opioid withdrawal itself can induce seizures, particularly if withdrawal symptoms are severe and include rapid changes in blood pressure, dehydration, or extreme agitation. If Contrave is taken by someone who is physically dependent on morphine, the risk of seizure activity may be even higher due to a combination of withdrawal effects and bupropion’s pro-seizure potential.
To minimize risk:
- Do not suddenly stop drinking alcohol while taking Contrave, as alcohol withdrawal can also increase seizure risk.
- Avoid other medications that lower the seizure threshold, such as certain antidepressants, tramadol, or high doses of stimulants.
- Tell your doctor if you have a history of head injury, seizure disorder, or eating disorders before taking Contrave.
5. Liver Health Considerations
Both naltrexone and bupropion undergo hepatic metabolism, meaning that liver disease can impact how these drugs are processed, potentially leading to systemic exposure and increased risk of toxicity. (NCBI).
Individuals with moderate to severe liver disease should avoid Contrave treatment, as impaired liver function may cause the medication to accumulate in the body, leading to higher-than-intended doses and increased side effects.
Additionally, morphine is metabolized primarily in the liver and kidneys, meaning that individuals with liver disease or renal impairment may experience longer drug half-life and stronger effects, including an increased risk of respiratory depression and serious injury due to prolonged sedation.
To ensure safety:
- Tell your doctor if you have liver disease before taking Contrave.
- Monitor liver enzymes regularly if prescribed Contrave treatment while having a history of liver conditions.
- Avoid high-fat meals, which may increase bupropion’s systemic exposure, leading to enhanced drug effects.
- Use alternative pain management methods if opioid medications are necessary.

Safety Recommendations
1. Comprehensive Medication Review
Before starting Contrave treatment, it is essential to provide a complete list of all medications—including prescription drugs, over-the-counter medications, herbal preparations, and dietary supplements—to your healthcare provider. This step ensures that potential drug interactions can be identified early, reducing the increased risk of complications such as opioid withdrawal, high blood pressure, and serious allergic reaction.
For example, individuals who are already taking opioid medications for severe pain may face serious issues if they start taking Contrave, as naltrexone will block opioid effects and could lead to withdrawal symptoms. Additionally, certain other medications, such as monoamine oxidase inhibitors (MAO inhibitors) used for depression or mental illness, can dangerously interact with naltrexone and bupropion, leading to conditions like serotonin syndrome or severely high blood pressure. (FDA)
To ensure safety, individuals should tell their doctor if they are taking:
- Opioid medications, including morphine, oxycodone, fentanyl, or tramadol
- Antidepressants like Lexapro, or mood stabilizers, particularly MAO inhibitors
- Medications like propranolol for high blood pressure or cardiovascular conditions
- Other weight loss medications or stimulants
- Drugs for mental health conditions, including treatments for bipolar disorder
- Over-the-counter drugs such as NSAIDs, cough suppressants, and decongestants
- Herbal preparations that could interfere with liver metabolism
2. Avoidance of Opioid Use
Because Contrave contains naltrexone, an opioid antagonist, it completely blocks the effects of opioids. Patients undergoing Contrave treatment should avoid using opioid-containing medications to prevent opioid withdrawal and ensure that the weight loss regimen is effective.
Even if a person is not currently dependent on opioids, using morphine or other opioid pain relievers while taking Contrave may still lead to unexpected complications. In emergency situations where opioid pain relief is necessary (such as following dental surgery or a serious injury), the healthcare provider may need to adjust the treatment plan by either:
- Temporarily stopping Contrave before opioid administration
- Using non-opioid pain relief alternatives, such as acetaminophen or NSAIDs
- Monitoring patients closely for signs of opioid withdrawal or pain management failure
Patients considering Contrave treatment should ensure they have been opioid-free for at least 7–10 days before starting the medication. (NIH) If there is uncertainty about past opioid use, a urine drug test may be performed before prescribing Contrave.
3. Regular Monitoring
Due to the potential side effects of naltrexone and bupropion, regular monitoring by a healthcare provider is essential while taking Contrave.
Key aspects of monitoring include:
- Blood Pressure Checks – Bupropion can increase blood pressure, so individuals with high blood pressure or cardiovascular morbidity should have regular readings taken. In some cases, additional medication adjustments or lifestyle modifications may be needed to prevent complications.
- Mood and Mental Health Assessments – Taking Contrave can lead to suicidal thoughts, false beliefs, or worsening mental illness, particularly in individuals with bipolar disorder or depression. Any signs of hallucinations, agitation, or mood instability should be reported to a healthcare provider immediately.
- Metabolic and Liver Function Tests – Because Contrave treatment affects liver disease and metabolism, routine liver enzyme tests may be required, particularly in individuals with a history of hepatic impairment or those who drink alcohol regularly.
- Weight Loss Progress—Patients using Contrave for chronic weight management should track their weight changes, ensuring that the medication is effectively helping them lose weight in combination with a reduced-calorie diet and physical activity.
Dr. Matthew Olesiak states, “Ongoing monitoring while taking Contrave ensures that potential risks—such as changes in blood pressure, mental health, or liver function—are managed before they escalate into serious complications.”
4. Patient Education
Patients should be fully informed about the potential risks and side effects of Contrave treatment, including:
- Recognizing signs of opioid withdrawal – Symptoms such as trouble breathing, eye pain, chest pain, or severe nausea could indicate withdrawal triggered by naltrexone. (FDA)
- Understanding the risks of low blood sugar—Contrave can contribute to low blood sugar, particularly in individuals with diabetes or those using other weight loss medications. Symptoms such as dizziness, confusion, or unusual sweating should be reported immediately.
- Identifying early signs of serotonin syndrome – A potentially life-threatening condition that can occur when bupropion interacts with certain other drugs (such as antidepressants or migraine medications). Symptoms include rapid heart rate, agitation, muscle stiffness, and high fever.
- Monitoring for allergic reactions—Some individuals may experience a serious allergic reaction while taking Contrave, such as rash, swelling, difficulty breathing, or anaphylaxis. If this occurs, seek immediate medical attention.
Patients should also be advised never to suddenly stop drinking alcohol while taking Contrave, as alcohol withdrawal combined with bupropion could increase the risk of seizures or severe mood changes. (NIH)
By staying informed and communicating regularly with their healthcare provider, patients can ensure that their Contrave treatment remains safe and effective.
Frequently Asked Questions (FAQ) About Contrave and Morphine
Understanding the potential interactions between Contrave and morphine is crucial for those using these medications. Since Contrave contains naltrexone and bupropion, it can significantly impact the effects of opioid medications like morphine.
Below are answers to common questions regarding the safety, risks, and recommended alternatives when taking these drugs together.
1. What medications should not be taken with Contrave?
Several medications should not be taken with Contrave, as they can lead to serious interactions or health risks. Opioid medications (such as morphine, oxycodone, and fentanyl) should be avoided because naltrexone blocks opioid receptors, potentially triggering opioid withdrawal. Monoamine oxidase inhibitors (MAO inhibitors), used to treat depression and mental illness, should not be combined with Contrave, as this could cause severely high blood pressure or serotonin syndrome.
Additionally, medications that lower the seizure threshold, such as other antidepressants, tramadol, or stimulant drugs, should be used with caution due to the risk of seizures. Check out our guide to see how Contrave interacts with other drugs.
Always tell your doctor about all prescription drugs, over-the-counter medications, and supplements before taking Contrave to prevent dangerous interactions. (FDA)
2. Can you take morphine while taking naltrexone?
No, morphine should not be taken while using naltrexone, as naltrexone is an opioid antagonist that blocks opioid receptors. This means morphine will not work to relieve pain, making it ineffective for treating moderate to severe pain.
Additionally, if a person is dependent on opioids, naltrexone can trigger sudden and severe opioid withdrawal, leading to symptoms such as nausea, vomiting, sweating, tremors, rapid heart rate, high blood pressure, and intense cravings.
Patients requiring opioid medications for pain relief should wait at least 7-10 days after stopping opioids before beginning naltrexone-based treatments like Contrave. (NIH)
3. What painkillers can I take with Contrave?
Since Contrave contains naltrexone, which blocks opioids, opioid-based painkillers (e.g., morphine, oxycodone, hydrocodone, and codeine) should be avoided. However, non-opioid pain relievers such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), and naproxen (Aleve) are generally safe alternatives for pain management while taking Contrave.
Some prescription nerve pain medications, such as gabapentin or pregabalin, may also be options for patients needing chronic pain relief. Before taking any pain relievers, consult your healthcare provider to ensure there are no additional risks based on your medical history.
4. What drugs cannot be taken with morphine?
Morphine should not be combined with medications that depress the central nervous system (CNS) or affect opioid metabolism.
Drugs to avoid include:
- Other opioid medications (e.g., oxycodone, codeine, fentanyl) due to overdose risk.
- Benzodiazepines (e.g., Xanax, Valium) and muscle relaxants, as they increase the risk of trouble breathing and life-threatening respiratory depression.
- MAO inhibitors, which can cause severe high blood pressure and dangerous CNS interactions.
- Certain antidepressants, which can increase the risk of serotonin syndrome.
- Alcohol, as it enhances sedation and may cause serious injury or death due to respiratory depression.
Always tell your doctor about all other medications before using morphine, as drug interactions can have severe and life-threatening consequences. (FDA)
5. What happens if you take opioids with Contrave?
If a person taking Contrave (which contains naltrexone and bupropion) also takes opioids, the opioid effects will be blocked, making them ineffective for pain relief. In individuals who regularly use opioids, this interaction can lead to sudden opioid withdrawal, causing symptoms such as nausea, sweating, anxiety, tremors, and severe flu-like discomfort.
This withdrawal can be dangerous and may require hospitalization if severe. Additionally, if someone attempts to take higher opioid doses to override the naltrexone block, this significantly increases the risk of overdose once naltrexone wears off.
If pain management is necessary while on Contrave, tell your doctor to discuss alternative treatment options.
6. Can you take bupropion and morphine together?
Bupropion and morphine should be used together with caution, as bupropion can lower the seizure threshold, and opioids like morphine may increase sedation and respiratory depression. Additionally, bupropion affects dopamine and norepinephrine, which could interact with morphine’s central nervous system effects, leading to unpredictable mood or neurological changes.
Patients with a history of seizures, head injury, or substance use disorder should be particularly cautious. While these two drugs are not always contraindicated, combining them should only be done under the supervision of a healthcare provider who can monitor for potential adverse effects.
Conclusion
The combination of Contrave and morphine presents significant interaction risks due to naltrexone’s opioid antagonism and bupropion’s effects on blood pressure and seizure threshold. Thorough communication with a healthcare provider is essential to navigate these risks effectively.
To ensure safe and effective treatment outcomes, patients should adhere to prescribed guidelines, report all medications and supplements they are taking, and attend regular medical appointments.
For more detailed information, consult the FDA’s prescribing information for Contrave and the NCBI’s LiverTox database on naltrexone and bupropion.